Clinical Reasoning in Low Back Pain
by Martin Krause
Clinical reasoning is the process by which the Musculoskeletal Physiotherapist assesses the client's dysfunction. Titled Australasian Musculoskeletal Physiotherapists are trained in the superior clinical reasoning skills required for independent self-directed reasoning. The cognitive and meta-cognitive skills required for clinical reasoning may lead to expertise if applied clinically for at least 10 years. This process not only allows the clinician to recognize their limitations, moreover it empowers the clinician to know how to plug any gaps in their knowledge by either researching a particular topic and/or attending post-graduate training courses (self directed learning). These skills are founded under the umbrella of life long learning (the 3 L's).
The following is an illustration of the process of clinical reasoning using the Maitland approach. This example, deliberately uses a reductionist approach to finding the 'comparable joint sign'. This example highlights the procedural reasoning aspects of the subjective and physical examinations. Maintaining a process, still allows the practitioner to involve themselves in deductive and inductive reasoning, whereby clarification is sought, whilst trying to establish a clinical picture. Sometimes, this is referred to as 'forward' and 'backward' reasoning, in order to verify that the information received from the subjective interview truly reflects the practitioners understanding of the presenting condition, which subsequently means that the physical examination can focus in on correlation between signs and symptoms. Care must be taken when using 'open versus closed ended questions' so that confirmation bias doesn't mire the clarity required for high quality predictive reasoning.
The 'experienced practitioner' will know what the 'end goal' looks like, whereas the 'inexperienced practitioner' can use the process to guide them through unfamiliar clinical terrain. Additionally, the process of collaborative reasoning with the client or with colleagues, can also lead to the experiential learning required to gain 10 000 hours of expertise. When psycho-social factors due to work related injuries, domestic abuse, political or religious abuse, or torture are involved a high level of ethical reasoning needs to be applied. Even in situations where children are participating in high level sport and parents, clubs or coaches are placing pressure on that child, high ethical principles need to be maintained, when making return to sport or work judgement calls. See : - Return to Sport : Delphi consensus RTS ACL and Post Concussion Syndrome elsewhere on this site.
Navigating through the clinical reasoning learning process can be very similar to navigating through terrain (in orienteering), where maps are used to form impressions of the physical surroundings, similarly 'mind maps' can be used to create flow diagrams of the cognitive processing, thereby 'bringing the subconscious into the conscious' through meta-cognition rather than innate luck. Examples of using 'mind maps' for various clinical presentations can be found in another section of this site.
The 'neurophysiology of treatment of low back pain using mechanical traction' could be an alternative treatment option to Fred's condition. Additionally, the importance of muscles and the immune system are discussed in a presentation on 'muscles as an organ of the immune system'.. The Geoff Maitland system uses oscillatory joint mobilisations as the primary treatment approach. In depth analysis of 'deterministic chaos and oscillatory systems are found here. Concepts of joint stability through oscillations are discussed elsewhere. Finally, how this approach has affected a 40 year career in physiotherapy can also be used to understand that this 'reductionist approach' can be a springing off point for profound reasoning, unexpected surprises and a fantastic journey through a career of ever evolving enlightenment.
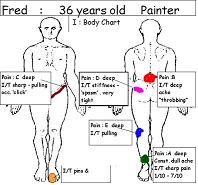
I: Body Chart
Relationships : -
Increase Pain A alone;
Increase Pain A with/without increase Pain B
- Increase Pain B + increase Pain D , and C
- can have increase Pain D and E without increase Pain A
- can have P+N / numbness without increase Pain BFrom the body chart what is your 'working hypothesis'?
Do you think there is more than one structure involved? Why?
Are there symptoms suggesting referred somatic or radicular pain? What are they?
II : Past History
nil history of Pain A prior to 6/12 ago
past history of Pain B over past 5 years
- onset after lifting a heavy load (~body weight) in a bent over position
- initial injury took 2-3 weeks to subside
- gradually worsening
increased frequency of Pain B (~ 2-3 times per year)
increased intensity of Pain B
takes longer to get better again ( ~ 4-6 weeks vs a few days)
takes less effort/strain for pain B to come on again
quality of pain B has changed from a 'dull ache' to a 'deep ache & throbbing'
past history of Pain C similiar to Pain B
- onset 5 years ago during the incidence of Pain B
- also gradually worsening , however the recurrences are not as frequent as Pain B
Pain D started at a similar time to pain A but is more frequent (almost constant tightness)
Pain E started some 2 years ago - insidious onset / little changed
history of recurrent sprained ankle on left.
unsure of onset of Pins and Needles / Numbness
previous physiotherapy treatment consisted of electrotherapy and massage and some exercises that helped
What information does the past history reveal w.r.t
- the relationships of the pain?
- your 'working hypothesis'?III : Current History
Pain A commenced 6/12 ago
- insidious onset that gradually worsened over the past few months
- started in the bottom of the heel and became greater in area and intensity.
- mostly constant pain since 2 months
- had been working a lot in the cold open air at the time of onset
- 3 week rest from running made little change
- 12 treatments from a Physiotherapist consisted of massage, ice and a stretching regime - has helped a little but did not last. Recommenced back exercises as Pain B had also been getting worse. Exercises consisted of 'modified' push ups and bring knee to chest whilst lying on back
What information does the current history reveal to help your 'working hypothesis'?
- central pain generating mechanisms? (neurophysiology)
-peripheral pain generating mechanisms? (neurophysiology and anatomical)
History of abuse, overuse, misuse?
IV Aggravating factors
- standing on a ladder for 30 minutes -> Pain A 3/10; Pain B 3/10
- can continue standing on ladder (risk of Pain C and D)
- standing and moving on ladder for 60 minutes -> Pain A 5/10; Pain B 2/10
- running 10km, the first few km?s are quite painful (~3/10) then it settles down to ~1/10, unless on uneven ground.
Easing factors
- After standing on the ladder for 60 minutes must stop activity, whereby Pain A decreases after approx. 30 minutes to 2-3/10. Pain B remains at 2-3/10.
- Stretching the 'Hamstring muscles' relieves Pain E somewhat.
- Extension exercises help Pain B, little effect on Pain A during day but good a.m.
- Brief (~ 5 minutes) icing of the heel helps Pain A when severe
- NSAIDS help Pain A a little with morning pain and stiffness
- Repeated or heavy (~10kg overhead) lifting may cause pain B
V : 24 hour behaviour
Morning
- the morning after running 10 km, when getting out of bed-> Pain A 7/10 ; stiff in region of pain B. Occasional Pain E.
- takes Pain A some 30 - 45 minutes to loosen up using a hot shower and stretches.
Evening
- both Pain A and Pain B can be worse if having spent a lot of the day climbing ladders;
- frequently Pain D is worse at the end of the day, as are the pins & needles
- running on even ground in the evening helps Pain B and Pain A after a period of time
Nocte
- pain A constant dull ache but better than during the day
- pain B wakes him occasionally. Unsure whether he wakes due to movement or due to positioning. Takes some 10-15 minutes to sleep again. Prefers to sleep on right side with the left knee up towards chest
- occasional calf cramps at night
- no pins and needles at night
What is the "irritability"? why?
What is the "Severity" ? Why?
What is the "Stage" of the disorder ? Why?
What is the "stability" of the disorder? Why?
Is there evidence for inflammation?
- neurogenic?
- non neurogenic?
- adverse neural tension?
How will you measure technique and treatment success?
Special QuestionsWeight loss OK; Steroids OK; Corda Equina OK; Cord OK; X-rays NAD; Operations OK; Other joints; OK Diabetes OK
VI: Physical Examination
|
|
|
|
|
|
||
Achilles : very tender to palpation, some rubifaction, some swelling, medial and lateral calf tightness
- : heel raise -> pain A 2/10, deviation into inversion.
Ankle : lateral instability
- : small big toe : Mortons Toe
Detailed information regarding the neuromodulation of pain as it relates to musculoskeletal physiotherapy
more clinical reasoning for the cervical spine-upper quadrant
Summary
Clinical reasoning for low back pain includes the following
-
Body Chart - one or more areas of pain
-
Past History - misuse (incorrect technique), abuse (trauma), overuse (prolonged activity), disuse (atrophy due to 'fear-avoidance' behaviour) leading to deconditioning and hence reduced loading tolerance increasing the susceptibility to recurrences even with minor loading activity
-
Current History - onset similar to past history, may be becoming progressively more frequent and more severe in nature, may be taking longer to settle than usual
-
Aggravating Factors - unguarded movements e.g. cough/sneeze, twist/turn; can move into every position but don't like to stay in any one position for too long, and have trouble moving out of that position
-
Special Questions - ask for X rays if you suspect spondylolisthesis due to Spina Bifida (patch of hair on back), or pars inter-articularis fractures; question steroid use, prostate cancer, blood anomalies, infections, major weight loss, cauda equina/cord compression symptoms, osteoporosis, etc
-
Physical Examination
Special Tests
- stork test
- walking + stair walking
- (dys)functional leg length discrepancy
- peripheral muscle length test on pelvic tilt (posterior tilt for rectus femoris, posterior tilt for hamstrings, and Thomas test)
- timing of peripheral muscle activation e.g. Gluteals vs. Hamstrings vs. Quadriceps
- Transverse Abdominal/Internal Oblique activation with leg and arm movements
- effect of changes in Latissimus Dorsi length on lumbar stability
- position of the Belly Button
- active straight leg raise for symphasis pubis instability/oblique abdominal muscle insufficiency
- multifidus activity and lumbar stability in
- prone lying hip extension (legs over end of bed)
- 4 point kneeling crossed extension
- rocking side to side and forward/backward, as well as alternating arm movements at 90 degrees flexion
- clunk test' in side lying
- after PPIVM's the movement pattern of restriction or excessive mobility may change dramatically
- spasm during PAIVM's
- Pressure Cuff biofeedback (inability to maintain the neutral zone)
- Transverse/Internal Oblique and Multifidus with EMG testing (no onset, late onset, or prolonged onset?)
Cognitive processes in clinical reasoning
Explanations and References
Terapia Manual y dolor (Castellano)
Dolor y Inflammacion (Castellano) PDF
Manual Therapie in der Behandlung von Schmerzen (Deutsch)
Tratamento do dor e inflamacao com fisioterapia manipulativa (Portuguese)
The importance of motor learning in the development of the concept of stability (English)
Exercises in map reading for enhanced cognition (forward thinking - predictive reasoning) (English)
Manual therapy in the treatment of pain and inflammation (English)
Nutritional Supplementation in endurance sport
Exercise and the Immune System (English)
Exercise and Type 2 Diabetes (English)
Exercise and Sarcopenia (English)
Fibromyalgia (English)

Examples of the assessment process for clinical reasoning
Beispiel von Klinisches Denken (Deutsch)
Clinical Reasoning Exercise for low back and lower Limb
Clinical example of treatment for functional instability and radicular LBP
A floppy feeling stiff - accompanied by visceral dysfunction - CREST syndrome
Cyclist riding fixed gear with an overactive right iliopsoas and left knee dysfunction
Multifidus dysfunction - a role for examination of the immune response?
Clinical Reasoning for prevention of cramps in a Triathlon
Presentation at the Rome conference in October 2005
Clinical Reasoning Exercise for Neck-Upper Limb
Pelvic floor and pudendal nerve pathology
Development of the concepts of stability
Shoulder instability and "tennis elbow"
Apresentacao Clinica e Perguntas
(RACIOCINIO CLINICO) (Portuguese)
Pattern recognition
Ultimately, the clinical reasoning process can be divided into a process of confirmation or negation either through positive diagnostic testing (eg Faber's test, Speed's test etc etc) with their inherent problems of validity and reliability or the process can involve treating a structure and evaluating the outcome by re-examining both the impairment and disability issues which the client presented with. The clients cognitive-linguistic appraisal of outcome can also be evaluated through the re-evaluation of the significant findings from the subjective examination.
Mind maps are a useful guide for the experienced clinician as they not only chunk together information but also provide a sequential structure for processing multiple information. Mind maps can provide a useful schemata for 'brain storming' and lateral thinking. Furthermore, mind maps provide a useful clinical aid to explaining cause and effect to the client, particularly when multiple sites of pain are present. Links to mind maps of some clinical conditions
- tennis elbow
- anterior hip pain
- hamstring injuries
- pelvic neck dysfunction in a cyclist
- Upper Cervical Spine Structural Instability
- Nutritional considerations and cramping in triathlon
- Knee pelvis back dysfunction in a runner with overactive Transverse Abdominus
- arm pain from L5 IVD hernia (with reference to FBL and Susanne Klein Vogelbach)
- pins and needles, numbess in cyclists feet - including biomechanical & vascular compromise
- carpal tunnel syndrome from upper cervical spine dysfunction? - including biomechincal & vascular compromise
- Gastrocnemius tightness - including biomechanics (inverse dynamics, young's modulus, kinetic energy)

The essence of clinical reasoning
As the physiotherapist gains clinical expertise their predictive reasoning or forward thinking should improve. The majority of our cognitive processing occurs in our subconscious whereby routines only change when their is a variation to our expectations. As such, the repeatedly rehearsed, systematic and structured clinical reasoning routine allows for cognitive efficiency. The experienced clinician can 'chunk' clinical patterns into recognizable objects, whereby many variables can be grouped into a meaningful piece of information. Since, the conscious brain can only process one piece of information at any one time, and only hold 6 pieces of information in short term memory, the reduced cognitive demands of 'chunking' allows the experienced clinician to increase the scope of their clinical expertise. Particularly, in more complex multi-dimensional musculoskeletal problems the Musculoskeletal Physiotherapist should be able to apply a multi-dimensional treatment approach. The discerning Musculoskeletal Physiotherapist uses correlations between disability measures with impairment measures such as restrictions in motion, altered form & force closure, inefficient force transmission, as well as cognitive behavioural factors to ascertain whether they are dealing with a familiar or unfamiliar 'clinical pattern'. The validity of each treatment technique is ascertained by their impact on disability and impairment measures. Predictive reasoning and a successful outcome confirms already established 'clinical patterns' or allows for the recognition of a new 'clinical pattern'. This new 'clinical pattern' can then be laid down into the long term memory and be used by the more efficient subconscious reasoning at a later date. Thus, similar to a 'grand master' chess player recalling thousands of strategic moves from famous games, the experienced clinician can recall clinical patterns and the processes needed to confirm these patterns in an efficient manner.
More precise research and formulation of clinical reasoning concepts has come from Mark Jones and his collaborators, in South Australia. Categories of reasoning which an experienced clinicians undertake include
-
Diagnostic reasoning
-
Narrative reasoning
-
Procedural reasoning
-
Interactive reasoning
-
Collaborative reasoning
-
Reasoning about teaching
-
Predictive reasoning
-
Ethical reasoning
Hereby, they have presented arguments for undertaking research paradigms which provide evidence for the superiority of this approach over protocol recipe based approaches. Moreover, the clinical reasoning approach supports/validates the use of techniques which improve disability and impairment measures. Hence, the physiotherapist and client can achieve immediate gratification when improvements are demonstrated. Similarly, if improvements are not forthcoming, then the process allows analysis and re-analysis (cognition and meta-cognition) of strategies already undertaken and rational decisions can be made because of the systematic nature of this approach. Thus, both the client and physiotherapist can actively learn during this process.
Uploaded : 14 November 2012
Updated : 2 February 2022