- the use of a pain diary for goal setting, clinical reasoning and the assessment of functional outcome in Musculoskeletal Low Back Pain
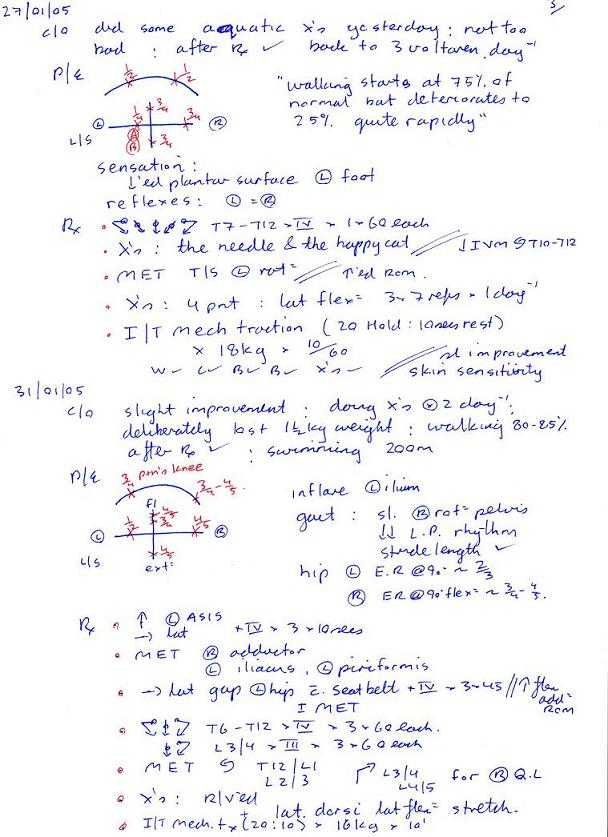
The following represents an interesting clinical reasoning scenario, whereby it was important to monitor and treat the neurological signs and symptoms, treat the cause of symptoms i.e. thoracic spine stiffness, functional pelvic instability and disc prolapses, as well as set realistic and functionally related exercise goals. Although, I don't regard my management of this condition as unique or outstanding, it did highlight the importance of listening and interacting with the client. In this case the client spontaneously began an excel spreadsheet which they used to monitor progress. It represents a great example of client initiated cognitive behavioural therapy, as well as a beautiful example demonstrating the relationship between clinical goals and functional goals.



Mechanical Traction for Low Back Pain





What is highlighted here, is the frequent change of side of 'upslip' in the pelvis, as well as alterations in direction of T/S mobility. In cases where clear cut neurological signs and symptoms can be assessed and used to validate the efficacy of treatment, these should be used to decide the dose and type of of treatment. However, where functional instability exists, general functional and pain intensity trends should be used to assess efficacy. Traditionally, Visual Analogue Scales (VAS) have been used to assess aggravating and easing factors. However, in conjunction with a functional activity scale the VAS can be used to determine the pain modulating capacity of the person. It would make sense that by generating such charts, the motivational-affective aspects of pain modulation may be encouraged.
Where no 'red flags' exist, a push currently exist to adopt protocol driven treatment approaches to non-specific low back pain (NSLBP) (Swinkels et al 2005). The strict definition of NSLBP is the inability to image a site of pathology. In this case the client had 'red flags' associated with marked disc pathology, however biomechanical generators of dysfunction from the pelvis and T/S were not imaged. Yet, using specific treatment to address these structural issues as well as engaging the client in the clinical reasoning process by validating each and every technique resulted in the generation of very interesting graphs which showed day to day variation, but more importantly demonstrated the general positive trend in treatment outcomes. The clinical reasoning process allows for a unique educational experience between the client and practitioner. Additionally, from the medico-legal point of view of 'informed consent' it actively involves the client in decision making. This process of assessing in-session and between-session changes in signs and symptoms has recently been validated by Tuttle (2005) for cervical spine pain. By promoting protocol based approaches to treatment, an element of safety for clients in the hands of inexperienced practitioners may be promoted, as well as reducing the risk of client dependency. Yet, the progressive and continuous assessment of signs and symptoms would appear to be a far safer approach to determining efficacy and safety. Additionally, by removing the need to discover unique and specific management of each and every clinical reasoning scenario a circular argument exists, in that a regimented-protocol-based-approach could reduce professionals to technicians when opportunities for promoting practitioner self-actualisation and excellence are removed. Therefore, countries like Australia, where primary practitioner status has existed for over 2 decades, graduate qualifications in musculoskeletal physiotherapy as well as specialisation will continue to be advocated.
Tuttle N (2005) Do changes within a manual therapy treatment session predict between-session changes for patients with cervical pain? Australian Journal of Physiotherapy, 51, 1, 43-48.
Swinkels ICS, van der Ende CHM, van den Bosch W, Dekker J, Wimmers RH (2005) Physiotherapy management of low back pain: Does practice match the Dutch guidelines? Australian Journal of Physiotherapy, 51, 1, 35-42.
Referred and interactive low back pain
Political role of clinical reasoning vs protocol based treatment repertoires
Last update : 20 January 2007


























































































































