What is glucose intolerance and how do muscle contractions affect type II diabetes?
by Martin Krause (2009)
-
26% of the population has glucose intolerance
-
since the 1980's there has been an increased prevalence of type II insulin resistant diabetes from 5.3% to 8.2% (1976 ->2002) to 9.3% (2006) (Gregg et al 2004; Cowie et al 2006 in Gregg & Kriska 2008)
-
many people do not know that they have diabetes let alone impaired glucose tolerance
-
glucose intolerance and type II diabetes is occuring in ever younger populations
-
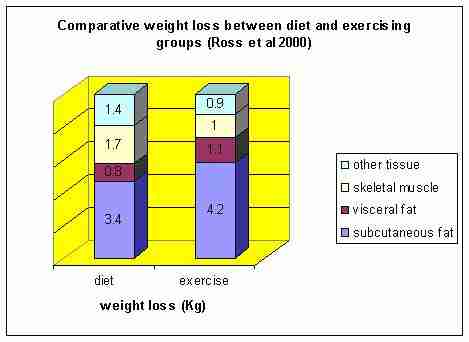
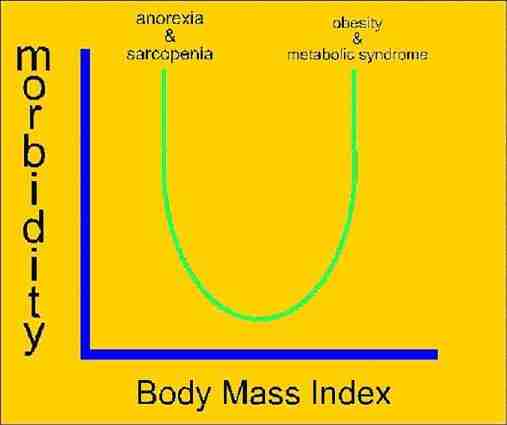
abdominal fat (as opposed to subcutaneous fat) is a major determinant in the development of glucose intolerance
-
two mechanisms for the development of type II diabetes from glucose intolerance are due to the lack of translocation of the Glut 4 receptor from the centre of the cell and the increased ability of long chain fatty acids to cross the cell membrane (due translocation of subcellular FAT/CD36 to the sarcolemma). Rather than being used correctly as an energy substrate (Beta Hydroxylase cycle) the fat is stored inside the cell as triacylglycerol (TAG) depots
-
the cells are clogged up by fats (increased TAG depots and reduced FAT/CD36 pool) analogous to a sticky date pudding
-
physiological, biochemical, and molecular evidence has shown that fatty acid movement across the plasma membrane is regulated acutely by muscle contraction, AMPK activation and selected hormones (insuline, leptin, resistin) as well as chronically by altered muscle contraction (Bonen Chabowski Glatz & Luiken 2008)
-
In insulin-resistant muscle, rates of long chain fatty acid (LCFA) transport are increased, which in turn leads to insulin resistance
-
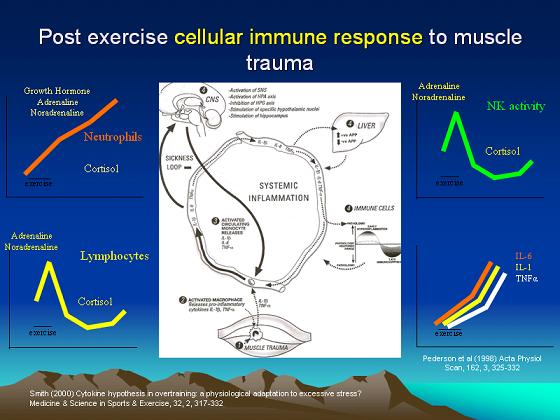
inflammatory - immune compromise may be an aspect in the development of type II diabetes
-
obesity-linked type II diabetes is associated with cytokine acute phase/stress response (White & Marette 2008)
-
levels of C-reactive Protein (CRP), a marker of low grade inflammation and acute phase protein response are elevated in children associated with higher adiposity (fat) (Cook et al 2000 in White & Marette 2008)
-
elevated levels of interleukin -6 (IL-6) and Tumor Necrosis Factor aplha (TNF alpha) and overexpression of interferon gamma (IFN gamma) in tissues of humans and animals with obesity has been observed (Yudkin et al 1999, Hotamisligil et al 1993, Perreault & Marette 2001 in White & Marette 2008).
-
muscles act as a sink for the action of insulin. Muscles acount for about 85% of insulin stimulated blood glucose clearance (DeFronzo et al 1981 in Cartee 2008)
-
muscles act as 'zeitgeber' (time keeper) on the circadian rythm affecting metabolism of blood sugars as well as the mobilisation of fat
Schroder and Esser (2013) Ex Sp Sc Rev, 41, 4, 224-229
-
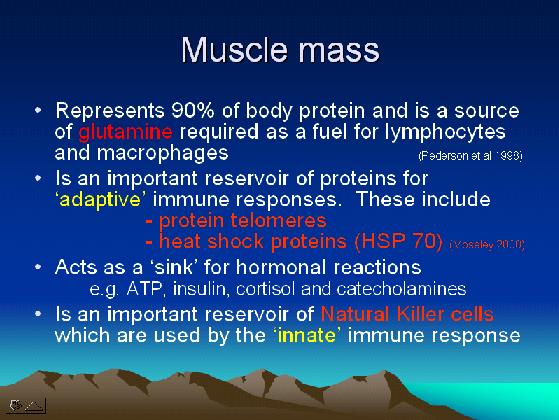
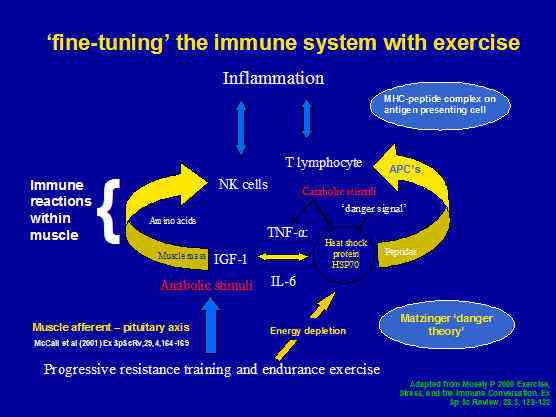
muscles are an important source of protein for the immune system
Marathon runners have a lower prevalence of hypertension, hypercholesterolemia, and diabetes. (Williams 2009, Med Sc Ex Sp, 41, 3, 523-529)
What can be done about glucose intolerance, type II diabetes and inflammation/immune function?
Exercise
-
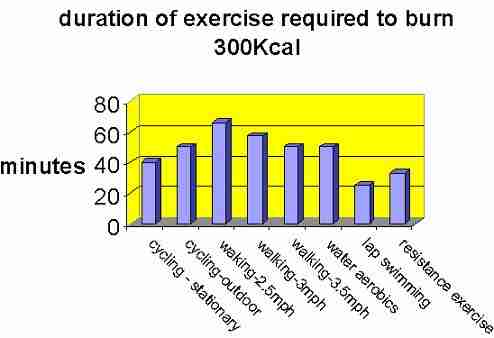
weight reduction through exercise (minimum of 700Kcals per day) and diet
-
training must include 6-8 exercises of large muscle groups of moderate intensity (70%Vo2max; RPE 14-17), 3-6sets x 10-15reps
-
must include abdominal girth reduction exercises
-
ideally some form of exercise daily eg squats, push ups, pull ups, abdominal strengthening (5-10minutes)
-
resistance training 1-2 x per week
-
endurance training (40-60minutes) 2-3 x per week
-
stress reduction stretching, meditation and/or yoga at least once per week
-
Cellular stress and eccentric contractions activate MAP kinase signalling which affect MSK 1, p90rsk and p38. The latter durectly affects Nuclear Respiratory Factors (NRF)1/2 which influences Mitochondrial biogenesis and the electron transport chain, Estrogen related receptor (ERR) alpha and the fatty acid uptake and oxidation as well as affecting Peroxismoe Proliferator-Activated Receptors (PPARs) and High Density Lipoprotein (HDL) synthesis
-
Motor nerve activity affects Calcium-dependent signalling, Ca-calmodulin which affects Myocyte Enhancer Factor (MEF) 2, activating Myosine Heavy Chains (MHC) and Glut 4 expression.
-
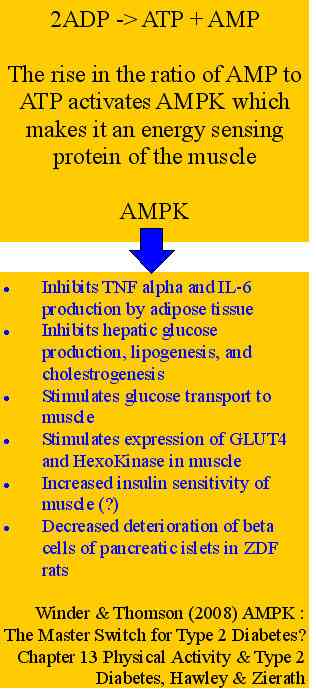
Energy status affects AMP-dependent signalling increasing AMP or decreasing ATP, AMPK and the expression of PGC1 (Peroxisome Proliferator-activated receptor gamma coactivator 1) which influences PPARs and HDL synthesis (Kraemer & Krook 2008)
-
Exercise leads to an insulin independent translocation of GLUT4 to the cell surface and an increase in glucose transport (Douen et al 1990; Lund et al 1995 in Kraemer & Krook 2008). Transgenic mice which over-express GLUT4 in adipose and skeletal muscle exhibit improved oral glucose tolerance and insulin-stimulated glucose disposal (Deems et al 1994; Liu et al 1993; Ren et al 1995 in Kraemer & Krook 2008). MEF2 and GLUT4 Enhancer Factor (GEF) have been implicated in this process via possibly AMPK and p38 MAPK (Kraemer & Krook 2008)
-
Endurance exercise has been shown to be of greater benefit than strength training in treating type 2 diabetes due to improved oxidative capacity through increased mitochondrial density.
-
PPARs are activated by dietry lipids and are therefore considered to be nutritional lipid sensors and to control lipid homeostasis (Smith & Muscat 2005). PPARs have also been implicated in mechanisms that release anti-inflammatory factors or repress the inflammatory response (Lee et al 2003, Pascual et al 2005 in Kraemer & Krook 2008)
-
PPARdelta has been shown to increase significantly in patients with type II diabetes following a 4month low intensity exercise program (Fritz et al 2006 in Kraemer & Krook 2008). This also correlated with improvements in other key clinical parameters.
see : Exercise and Sarcopenia
Polycystic Ovary Syndrome (PCOS)
PCOS is associated with increased risk of several metabolic complications including insulin resistance, type II diabetes, dyslipideamia, and possibly cardiovascular disease. The increased incidence was thought to be the result of small, dense LDL. In other populations with cardiovascular disease and insulin resistnace, similar sublcass annomalies have been found, as well as increased concentrations of large VLDL and small LDL particles and decreased numbers of large HDL particles. Larger VLDL size and smaller HDL size were also shown to be strongly associated with the development of type II diabetes.
Investigations prior to 2009 which did not use nuclear magnetic resonance (NMR) found little correlation between exercise and improved blood particle outcome. However, investigations using a protocol of Studies Targeted Risk Reduction Interventions through Defined Exercise (STRRIDE) with NMR. Brown et al (2009) used an 8-12 weeek ramp-up protocol followed by 12 weeks of moderate intensity (calorific equivalent to walking 12miles/wk) in 8 premenopausal women. Their results demonistrated significant reductions in concentrations of large VLDL/chylomicrons and medium/small HDL and increased large HDL and average HDL size in the exercise group compared with controls. These results represent a good investment for the 3h24min per wek needed for this intervention.
Brown et al (2009) Med Sci Sp Ex, 41, 3, 497-504S
Fine tuning the body with exercise and diet

1 calorie = 4.184 joules
-
Insulin sensitivity can be incresed after a single bout of exercise which is not attributable to reduced body fat
-
Reduced muscle triglyceride concentration is not essential for improved insulin sensitivity with dietry or exericise intervention strategies. In fact with endurance exercise the intramuscular triglyceride concentrations can increase.
-
Calorific restriction neither activates AMPK nor does it trigger GLUT4 abundance, in contradistinction to what occurs with exercise training (Zheng et al 2001; Cartee et al 1994; Gazdag et al 2000 in Cartee 2008)
-
Insulin and exercise use distinctly different pathways to induce GLUT4 translocation from the cytoplasm to the cell surface (Hooloszy & Hansen 1996 in Cartee 2008). Contraction dependent GLUT4 translocation appears to require elevated Calcium and elevated AMPK levels (Mu et al 2001; Wright et al 2004 in Cartee 2008)
-
After 7days of Calorific Restriction (CR) (consuming 800kcal/day) participants lost 2.2kg (17% of total weight) but they achieved 45% in insulin sensitivity measured at 3months of CR (Kelley et al 1993 in Cartee 2008). CR in obese humans with type 2 diabetes demonstrated weight loss of only 3.5% but this was accompanied by a 35% increase in glucose disposal rate during a hyperglycemic clamp (Aciero et al 1999 in Cartee 2008). Clearly, modest weight loss can be accompanied by marked improvement in glucose tolerance
-
GLUT4 abundance is not affected by CR (Cartee 2008) suggesting that CR may enhance glucose transport by acting specifically on the insulin signaling pathway
-
As of 2008, the results of combined exercise and CR on insulin sensitivity and hence glucose tolerance have yet to be determined.
However, continued compliance over time seems to be a major issue when it comes to exercise regimes
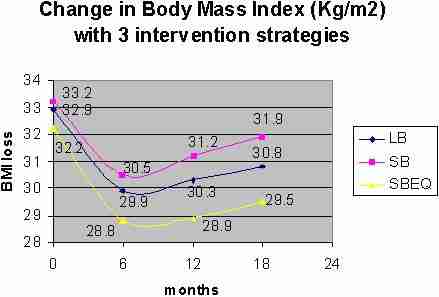
High intensity exercise (RPE 15.4) versus low intensity exercise (RPE 11.1) for a 16 week walking programm was shown to reduced regional body fat by 47 vs 11cm2 and abdominal visceral fat content by 24 vs 7cm2 (Irving et al 2008) . Further reductions in visceral fat were reported by the same authors with 8 months of vigorous jogging (~20miles/week). This is significant as visceral fat is directly correlated with the progression of glucose intolerance to type II insulin resistant diabetes. Interestingly, moderate intensity exercise (500Kcal) energy expenditure was shown to improve postprandial dyslipidemia in people diagnosed with metabolic syndrome (Mestek et al 2008). This finding wasn't found in healthy subjects, suggesting that even moderate amounts of activity can have large impacts on a critical risk factor for morbidity.

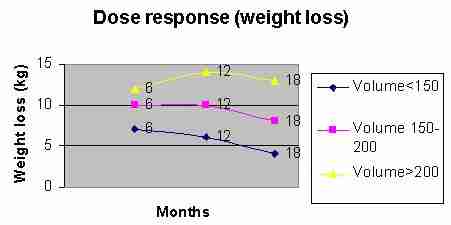
A dose - response effect has been observed during progressive exercise. Notably, even a small exercise dose of 400Kcal/week (40-50% of recommended guidelines) results in a significant improvement in insulin sensitivity (Dube et al 2012, Med & Sc in Sp & Ex, 44, 5, 793-799)
See : Exercise Training and Weight Loss
Minimal difference between aerobic and progressive resistance exercise on metabolic profile and fitness in older adults with diabetes mellitus: a randomised trial.
Ng CLW, Goh SY, Malhotra R, Østbye T, Tai ES (2010) Journal of Physiotherapy 56: 163–170
Question: Is progressive resistance training as effective as aerobic training of similar duration in sedentary older adults with diabetes mellitus?
Design: randomised trial with concealed allocation, assessor blinding and intention-to-treat analysis.
Participants: Sixty people with Type 2 diabetes mellitus with glycosylated haemoglobin (HbA1c) between 8% and 10% in the past month.
Intervention: One group undertook progressive resistance exercise and the other group undertook aerobic exercise. Both groups completed 18 sessions over 8 weeks. In each session, the progressive resistance exercise group did nine resistive exercises while the aerobic exercise group did 50 minutes of aerobic exercise.
Outcome measures: HbA1c, blood glucose, lipid profile (total, high- and low-density cholesterol and triglycerides), weight, body mass index, body fat, waist circumference, waist:hip ratio, blood pressure, and peak oxygen consumption.
Results: Forty-nine (82%) participants completed the intervention. HbA1c reduced by a similar amount in both groups (MD 0.1%, 95% CI –0.3 to 0.5). However, significant between-group differences occurred in change in waist circumference in favour of progressive resistance exercise (MD –1.8 cm, 95% CI –0.5 to –3.1), and in change in peak oxygen consumption in favour of aerobic exercise (MD 5.2 ml/kg, 95% CI 0.0 to 10.4).
Conclusions: Progressive resistance exercise has similar effects to aerobic exercise and therefore offers a useful alternative for patients unable to participate in aerobic exercise. Trial registration: NCT01000519.
Diet
- reduce fat
- reduce suger - low GI
- pasta - al dente (the longer it boils the higher the GI)
- Suger Guard and Fat Guard tea
- low GI muesli and low fat yogart (check sodium {Na+} content - frequently it is very high and can lead to high blood pressure)
- nuts and seeds as nibbles
- don't overeat as calories in = calories out. Excessive calories are stored as fat
- monostaurated and polyunsaturated fats (check the label - even olive oil may contain saturated fats or worse still trans fats)
- avoid animal fats
- fish, esp red fish such as salmon
- fresh fruit (most fruit is good however check GI charts eg watermelon is high GI)
- apple a day keeps the doctor away
- fresh vegetables
- legumes - Lentils, Cous cous, Chick peas, beans Baked beans and Kidney beans, etc
- oats and natural muesli (check GI and sodium content)
- Barley and Bulgur
- Breads made with wholegrain rye, barley, oats, soy with added sunflower and linseeds, or sourdough bread
- Wholemeal spaghetti
Supplements
-
Fish Oil (omega 3) - 1000mg daily
-
Cold pressed Flaxseed oil (omega-3, 6, 9) - good fats versus bad fats
-
Magnesium (esp if there is a blood pressure problem) - 300mg daily
-
Co-enzyme Q10 - for mitochondrial energy transfer
-
Vitamen B for the liver - energy power house of the body and hence metaboliser of glucose and producer of glycogen; Vit B6 50-100mg, Vit B3 500mg for one month and then 250mg daily
-
Vitamen C (1-2g) and Vitamen E (400-800IU) to prevent glycosylation
-
Chromium 250-500mcg daily
-
Curcumin - immune enhancer and anti-inflammatory derived from tumeric powder (Curcuminoids)
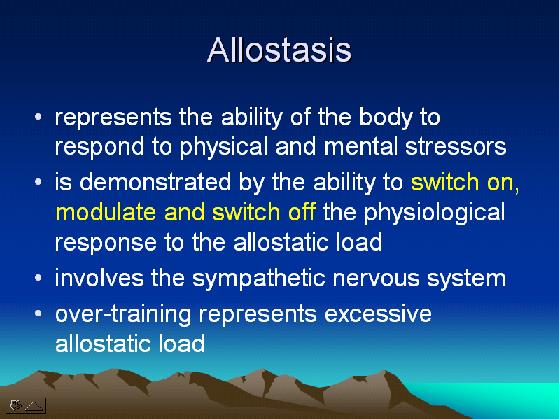
Stress and Allostasis
Stress affects blood sugar levels both directly and indirectly. Stress can cause an overproduction of hormones such as adrenaline and cortisol, which makes blood suger rise. In addition, people under stress tend to adopt unhealthy lifestyles, such as poor eating habits, smoking and alcohol which all have a negative impact on blood sugar. Cognitive behavioural approaches to stress managment, guided imagery, as well as yoga and meditation can all be used to eleviate stress.
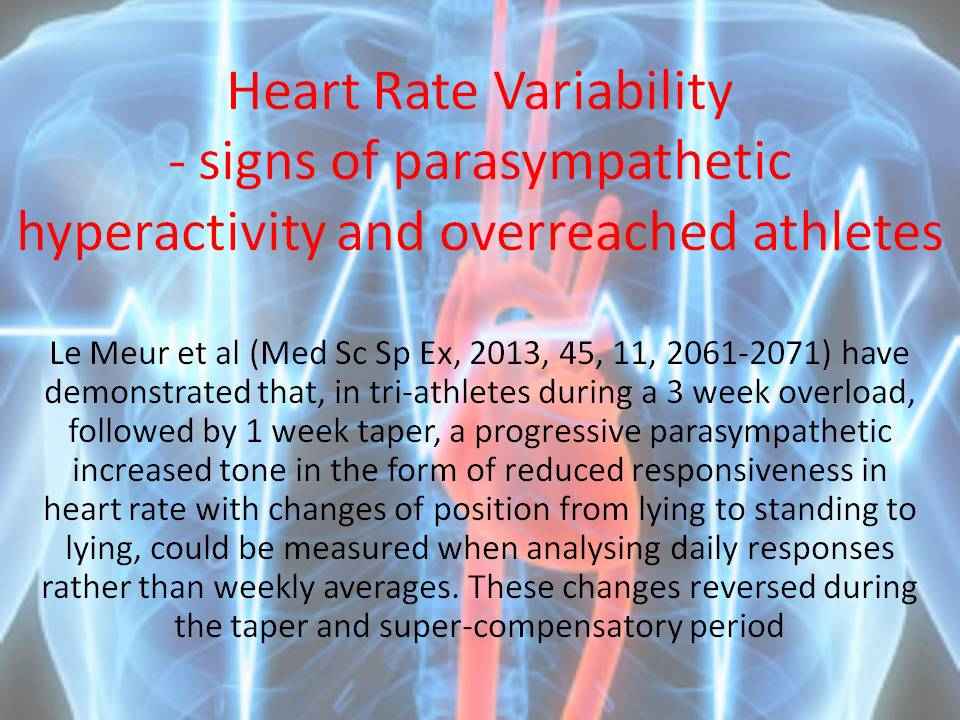
Exercise and heart rate recovery
Exercise and heart rate recovery has been demonstrated to be as sensitive marker to the balance between sympathetic and parasympathetic nervous system activity. Vagal tone and smpathetic-parasympatheic balance have long been associated as a fitness marker through reduced blood pressure and resting heart rate. Specifically, the initial post exercise plateau seen in fit individuals remains elevated in low fitness individuals despite low rates of oxygen consumption (HR/VO2plat). Yeckel et al (2009) concluded that heart rate recovery after exercise was a sensitive marker of this balance. Additionally, they concluded that this exercise recovery indiex for sympathetic overactivity was linked to insulin resistance (Yeckel et al, 2009, Med Sc Ex Sci, 41, 3, 505-515)
Clinical reasoning, the neuro-matrix and allostasis in explaining the role of musculoskeletal physiotherapy in health and disease
Macrophages are necessary for skeletal muscle regeneration. Pro-inflammatory macrophages stimulate myoblast proliferation, whereas anti-inflammatory macrophages stimulate their differentiation. Macrophages that invade skeletal muscle soon after injury present a specific phenotype, characterized by high expression of TNF-alpha, interleukin-1beta and secretory leukocyte protease inhibitor (SLPI). Non-phlogistic phagocytosis of the apoptotic and necrotic debris switches the phenotype of pro-inflammatory macrophages into anti-inflammatory macrophages. Consequently, there is a high expression of Transforming Growth Factor- Beta (TGF-beta), interleukin - 10 (IL-10), and peroxisome proliferator-activated receptor - gamma (PPAR-gamma) which have been shown to be associated with the resolution of inflammation and tissue repair (Chazaud et al 2009)
Cognitive Behavioural Therapy for exercise prescription

see : Neuro-immune and Cognitive Behavioural Response to Exercise
Tendonopathy
Gathering evidence suggests that tendonopathies are associated with disturbances in immune function and lipid metabolism (Prof George AC Murrell, Dr Stephen J O'Brien, 2011). Apart from the impact of diabetes on blood vessels and nerve fibres, there appears to be a direct relationship between metabolic syndrom and musculoskeletal dysfunction.
Hypertension
Some exciting research is suggesting that inspiration breathing against resistance can significantly reduce blood pressure.
An inspiratory load enhances the antihypertensive effects of home-based training with slow deep breathing: a randomised trial
Chulee U Jones , Benjarat Sangthong and Orathai Pachira
Khon Kaen University, Rangsit University Thailand
Question: Can adding an inspiratory load enhance the antihypertensive effects of slow breathing training performed at home? Design: Randomised trial with concealed allocation. Participants: Thirty patients with essential hypertension Stage I or II.
Intervention: Experimental groups performed slow deep breathing at home, either unloaded or breathing against a load of 20 cmH O using a threshold-loaded breathing device. Participants trained for 30 min, twice daily for 8 weeks. A control group continued with normal activities.
Outcome measures: Resting blood pressure and heart rate were measured at home and in the laboratory before and after the training period.
Results: Compared to the control group, systolic and diastolic blood pressure decreased signifcantly with unloaded breathing by means of 7.0 mmHg (95% CI 5.5 to 8.5) and 13.5 mmHg (95% CI 11.3 to 15.7), respectively (laboratory measures). With loaded breathing, the reductions were greater at 18.8 mmHg (95% CI 16.1 to 21.5) and 8.6 mmHg (95% CI 6.8 to 10.4), respectively. The improvement in systolic blood pressure was 5.3 mmHg (95% CI 1.0 to 9.6) greater than with unloaded breathing. Heart rate declined by 8 beats/min (95% CI 6.5 to 10.3) with unloaded breathing, and 9 beats/min (95% CI 5.6 to 12.2) with loaded breathing. Very similar measures of blood pressure and heart rate were obtained by the patients at home.
Conclusion: Home-based training with a simple device is well tolerated by patients and produces clinically valuable reductions in blood pressure. Adding an inspiratory load of 20 cmH O enhanced the decrease in systolic blood pressure. Trial registration: NCT007919689. [Jones CU, Sangthong B, Pachirat O (2010) An inspiratory load enhances the antihypertensive effects of home-based training with slow deep breathing: a randomised trial. Journal of Physiotherapy 56: 179–186]
References
Irving BA et al (2008). Effects of exercise training intensity on abdominal visceral fat and body composition. Medicine & Science in Sports & Exercise, 40, 11, 1863 to 1872
Mestek et al (2008) Aerobic exercise and postprandial lipemia in men with the metabolic syndrome. Medicine & Science in Sports & Exercise, 40, 12, 2105 to 2111
Uploaded 10 January 2009 ; Updated 23 September 2013