The important concepts of allostasis and exercise, in the immuno-humoral response, to cognitive environmental monitoring, when considering musculoskeletal dysfunction
written by Martin Krause, March - July 2005
B.Appl.Sc (Physio), M.Appl.Sc (Manip.Physio), Grad.Dip.Hlth.Sc (Ex & Sport), Grad.Cert.Hlth.Sc.Edu
Table of contents
Nitrogen Balance - catabolic versus anabolic considerations
Neuroimmune response to trauma
The sympathetic nervous system
Muscle, Liver, Kidney immune responses
Exercise and Delayed Onset Muscle Soreness (DOMS)
"Inflammaging" - effects of aging on eccentric exercise response
Adaptive versus Innate Immune Response
Abstract
A paradox exists whereby physiological systems activated by stress can not only protect and restore but also damage the body. Critical to survival is ‘allostasis', which is defined as “the ability to achieve stability through change”(McEwen 1998). Chronic overactivity or underactivity of allostatic systems can lead to dysfunctional responses by cytokines to trauma. The sympathetic nervous system (SNS) plays a central role in modulating cytokine release by communicating between the central nervous system (CNS) and immune system (Hasko 2001; Raison & Miller 2003). Altered SNS activity has been attributed with ongoing musculoskeletal pain in people with post-surgical failed back syndrome (Geiss et al 2005) and whiplash (Sterling et al 2005). Cytokines are the messengers of the ‘innate' immune system and are responsible for bi-directional communication between the body and the brain (Watkins et al 1995). An alternative ‘adaptive' immune system uses heat shock proteins (HSP) as a cellular link to mobilise T-lymphocytes and can be activated in response to heat, cold, metabolic stress and/or ‘danger and safety' signals (Moseley 2000; Watkins & Maier 2000). Since cytokines and HSP's are mobilised during moderately strenuous exercise, it is plausible that moderate intensity progressive resistance training (PRT) ‘fine tunes' neuro-immune stressor adaptation responses (Krause 2003). Furthermore, by enhancing lean muscle mass, the immune system has a greater reservoir of proteins to be used during inflammatory activity. Post-traumatic treatment interventions using cognitive behavioural therapy have been recently advocated to address motivational-affective and cognitive-evaluative aspects of pain modulation. When dealing with the stress of pain, it is conceivable that the necessary “danger and safety signals” required by the neuro-immune systems for allostasis can be incorporated into the clinical reasoning process whereby realistic and attainable functional exercise goals are defined through effective communication during client-practitioner interaction.
Introduction
In Australia, with a population of 19 million people, the treatment for chronic musculoskeletal disability alone costs $AUD4.7 billion annually. This figure does not take into account lost productivity to the community. Multi-modal treatment approaches for multifactorial musculoskeletal problems have recently been advocated which include traditional manual therapy, dry needling (intramuscular stimulation), acupuncture, muscle energy techniques, education, meditation and yoga as well as exercises for metabolic, co-ordinative and cognitive reasons. This has resulted from the gathering body of evidence which implicates the central nervous system (CNS) and peripheral nervous system (PNS) and immune systems in complex and dynamic neuro-immune interactions during activities of daily living.
Research into immunology has provided specific insights into understanding the role of the musculoskeletal system in immune defence, as well as the role of immune defence in musculoskeletal adaptation to training and injury. Importantly, the bi-directional signalling relationship of cytokines, between the locus of inflammation and the central nervous system (CNS) has been highlighted. Moreover, the recent understanding of the role of muscle mass as an important source of telomere proteins of eukaryotic carrier sites, for immune system mRNA splicing , should be of considerable interest to physiotherapists who regular prescribe exercise and advise on prophylactic health.
Figure 1 : Protein turnover and the prevention of negative nitrogen balance
However, sports scientists have also highlighted the paradox of post endurance exercise immune suppression, which has led to suggestions that this is due to the double jeopardy of relatively reduced energy supplies combined with musculoskeletal trauma from repetitive exercise (Fig 1 & 2). Whilst working with elite amateur and professional athletes in the late 1980's/early 1990's I noticed that they seemed to be particularly prone to musculoskeletal injuries such as stress fractures, opportunistic infections, and a multitude of symptoms, which could eventually lead to loss of performance and even chronic fatigue syndrome. Tragically, there were several incidences of sudden unexplained myopathic scarring leading to cardiac arrest & death amongst young elite Orienteers during this period. This lead me to conduct a literature review on neurohormonal systems and their relationship to musculoskeletal injury. Specifically, researchers were examining the superior cervical ganglion (SCG), the hypothalamic-pituitary-adrenal axis (HPA) : pro-opioimelanocortin, thyroid stimulating hormone (TSH), hypothalamic-pituitary-gonadal axis (HPG) : luteinising hormone and heat shock proteins (HSP's). Despite an obvious need to identify the causes of such phenomenology, the limited and predominantly animal research that existed during this time wasn't followed up by sports scientists for another decade.
Figure 2: Neuro-immune response to trauma
Mazinger's Danger Hypothesis and the 3 laws of lymphotics
Muscle provides an important source of heat shock proteins (HSP) for immune responses . Traumatic injury involves a signalling cascade whereby the release of inflammatory substances results in a counter-modulating process of containment. An inflammatory soup of histamines, prostaglandins, phagocytes, neurotrophic factors and cytokines localize the febrile response resulting in the release of heat shock proteins (HSP's). Little is known about HSP's, however they are likely to play a significant role in the containment of spreading inflammation and infection. These substances are activated in the presence of altered temperature, metabolic, mechanical and psychological stress and/or in the presence of a ‘danger signal'. Recently, Moseley (2000) highlighted Mazinger's danger hypothesis, which was formulated to understand the reason why some cell replication processes are recognized as alien whilst others go unrecognised (e.g. cancer). It consists of 3 laws of lymphotics for the ‘danger hypothesis' to work . T-lymphocytes need to receive 2 signals. The first signal is the binding of T-lymphocytes with a major histocompatibility (MHC) peptide complex on the antigen presenting cells (APC's). The second signal required comes from molecules on APC's. If this second signal isn't present then the T-lymphocyte undergoes apoptosis. Thirdly, if the co-stimulatory signal occurs then the T-lymphocyte is activated for a defined period during which time they can be activated by the MHC-complex alone. T cells activated by both the primary and co-stimulatory danger signals proliferate and become cytotoxic T lymphocytes (CTL's). Recent investigations have demonstrated that HSP's have a role in antigen presentation with resultant CTL activation. Additionally, the modulation of cytokine responses, by lymphocytes and macrophages, as well as acting as targets for NK cells, occurs when HSP 70 is expressed on the surface of tumor cells and virally infected cells. Notably, the HSP 70 subgroup, are found in abundance in skeletal muscle. Interestingly, HSP's have a similar structure to the MHC-complex, yet HSP's are intracellular proteins whereas the MHC-complex is both intra- and extracellular (i.e.trans-membranal). Therefore, HSP's are found extra-cellularly only when the cell has been exposed to a stress. Hereby, exposure of immune cells to HSP's, results in the proliferation of cytokines (Mosley, PL 2000). Hence, this theory suggests that all cells in the body are immune-competent and that antigen display in the absence of a ‘danger signal' results in tolerance. Muscle specific HSP70 can presumably be used by the immune system to regulate the fight against infection and inflammation.
The Sympathetic Nervous System
Energy requirements and sympathetic nervous system function are likely to directly influence immune responses. The sympathetic nervous system mobilises fat and carbohydrate, which is turned into working energy by muscle through the beta-hydroxylase and Kreb's cycles. In the presence of acute inflammation, the body will burn fat in preference to carbohydrate. An increase in gluconeogenesis occurs in the liver to maintain blood glucose levels for brain function. This process requires the proteins glutamine and alanine as the primary precursors for gluconeogenesis in the liver and are released from muscle (Wagenmakers 1998). The Hypothalamic Pituitary Adrenal (HPA) axis releases glucocorticoids, which act as muscle catabolic agents by mobilising the release of these proteins from muscle. Glutamine is essential for lymphocyte proliferation and macrophage function (Keast 1996) as well as acting as a precursor for inflammatory related liver proteins (Marks et al 1996). It has been argued that the HPA system may be modulatory when provided with the necessary cues that represent the ‘danger signals' and ‘safety signals' required to switch on and off the inflammatory-immune response (Moseley 2000). Alternately, circulating cytokines (IL-1) are thought to bind in the hypothalamus via vagal afferents (from the stomach) thus also potentially modulating these events (Waitkins & Maier 2000). Additionally, the locus coereleus and its noradrenergic sympathetic nervous system modulate spinal cord and cortical transmission of pain processing signals. Having this alternate pain suppression mechanism besides circulating opioids may be important for immune defence as increased blood opioid levels have been shown to suppress Natural Killer (NK) cell activity. Evidence for this was seen whereby the beneficial effects of peri-operative opioid analgesia on immune function contrasts with immune impairment when high doses of opioids are given to un-operated resting animals (Pain Clinical Updates: March 2005). Yet another aspect of the sympathetic nervous system, involving the Intermediolateral cells of the spinal cord, can sense and thereby modulate the relationship between pro and anti-inflammatory cytokines by virtue of the peripheral sympathetic nervous system's anatomical innervation of the dorsal root ganglion ( see Krause 1995 ) as well as it's innervation of other musculoskeletal tissue (Hasko 2001). This is important as these localized regulatory mechanisms involving pro-inflammatory and anti-inflammatory cytokines send signals to the CNS resulting in the assessment of the requirements for the containment of infection and inflammation as well as sensing the rate of recovery from the injury. However, in cases of trauma to the sympathetic ganglion, as after Whiplash, this modulatory mechanism could conceivably be compromised. Thus there are at least 4 SNS's all designed to deal with the containment of inflammation (fig 3 & 4). In the extreme case of traumatic inflammation and infection, if containment is unsuccessful then life threatening cachexia and sepsis may occur . It is plausible that meeting energy requirements through either dietary supplementation &/or SNS mobilisation is vital for optimal neuro-immune responses during and after exercise for the prevention of negative nitrogen balance (fig 1) as well as for sensing the status of inflammation.
Muscle, Kidney, Liver interactions during Immune responses.
Figure 3 Modulation of pain and inflammation by the sympathetic nervous system
Figure 4 Sympathetic modulation of the 'inflammatory soup'
Exercise and Growth Hormone
Bed rest can have deleterious effects on muscle function. Researchers have recently described a direct muscle afferent-pituitary axis whereby bio-assayable growth hormone (BGH) regulation is tightly coupled with muscle function rather than muscle fibre type. Unlike, exercise-induced increases in plasma immuno-assayable growth hormone (IGH), whose concentration peak occurs during or after longer duration aerobic or resistance exercise involving larger muscle mass, BGH is released after a brief series of isometric contraction (McCall et al 2001). The BGH response is absent , despite the maintenance of normal torque output and pre-exercise plasma BGH and IGH, when leg musculature is chronically unloaded, as after 2 days bed rest or space flight. They hypothesised that this was due to chronic alterations in proprioceptive inputs (McCall et al 2001). These responses normalised within approximately 8 days of ambulatory recovery. Furthermore, they suggested that BGH stimulates bone growth and that low threshold fibre activation through electrical stimulation, exercise and /or vibration may ameliorate the effects of chronic unloading (McCall et al 2001). Moreover, this is direct evidence for the existence of a muscle-pituitary functional pathway in the absence of inflammation. It also highlights the need not to underestimate the effects of bed rest when recommencing a training regime after a period of illness or trauma.
Exercise and DOMS
After intense eccentric and/or unaccustomed exercise athletes may experience the pain and inflammation associated with delayed onset muscle soreness (DOMS), which potentially reduces performance as well as compromises immune responses. DOMS is associated with the broadening and streaming of the Z-bands leading to actin-myosin de-coupling and the release of metalloproteinases (MMP's) (Lieber et al 2002, Kovanen 2001). Localized inflammation is necessary for growth, healing and repair after injury . It would appear that the balance between pro-inflammatory and anti-inflammatory cytokines determines this process. The evidence for this comes from research, which demonstrate low expression of MMP's in undamaged tissue. Their production is induced in response to cytokines, growth factors, and hormones in situations involving active tissue remodelling and cell migration, such as wound healing and inflammation involving extracellular matrix remodelling (Kovanen 2002). After heavy eccentric exercise induced DOMS, the muscles can require up to 28 days to recover (Lieber & Fridén 2002). The balance between stress and recovery defines a successful training regime (See Krause 2003 ). Therefore, goal oriented training regimes are an important system for positive muscle adaptation to take place, as it avoids overload and the potential loss of performance and immune compromise in the 28 days post intense eccentric exercise (fig 5).
Figure 5 Muscular-immune response to exercise
Macrophages are necessary for skeletal muscle regeneration. Pro-inflammatory macrophages stimulate myoblast proliferation, whereas anti-inflammatory macrophages stimulate their differentiation. Macrophages that invade skeletal muscle soon after injury present a specific phenotype, characterized by high expression of TNF-alpha, interleukin-1beta and secretory leukocyte protease inhibitor (SLPI). Non-phlogistic phagocytosis of the apoptotic and necrotic debris switches the phenotype of pro-inflammatory macrophages into anti-inflammatory macrophages. Consequently, there is a high expression of Transforming Growth Factor- Beta (TGF-beta), interleukin - 10 (IL-10), and peroxisome proliferator-activated receptor - gamma (PPAR-gamma) which have been shown to be associated with the resolution of inflammation and tissue repair (Chazaud et al 2009)
Effects of "inflammaging" on the inflammatory-immune-oxidative response to the Stretch-Shortening cycle
Age related differences have been demonstrated from stretch-shortening-contraction exercises. At day 3, muscles of young rats respond with a robust secondary response including an increase in interstitial space, cellular interstitium, muscle fibre degeneration, gene expression, and cytokine/chemokine protein levels, whereas old rats did not. Accompanying the lack of degenerative/regenerative response was a sustained force deficit. Additionally, oxidative stress-relevant pathways such as glutathione-mediated detoxification, GADD45 signaling, and nuclear factor mediated oxidative are high and remain unchanged with SSC injury exposure, whereas for young animals the REDOX environment is heightened by SSC-injury exposure and begins to return to normal physioolgical levels by day 10. The notion thus exists, that a timely secondary response is necessary for clearing sites of damage and attracting functional satellite cells for recovery. Cytokines, Interleukin-1 and 10 and chemokine ligand 2 (CCL2) are thought to play significant roles in the latter. Paradoxically, IL1 and IL10 and CCL1,2 and 3 have all been shown to be elevated 2-4 fold in elderly populations. Chronic subclinical inflammation and inflammatory signalling has been called "inflammaging". Manipulating exercise prescription by using SSC training only 2 versus 3 times per week was found to increase muscle mass, regardless of age. Thus, additionally recovery time results ina more favorable REDOX environment (Rader & Baker 2017, Exerc Sp Sc Rev, 45, 4, 195-200).
Adaptive versus Innate Immune Response and muscle mass
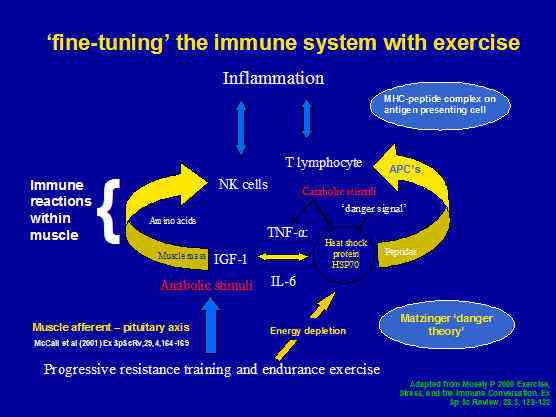
Microtrauma-induced inflammation, can result in the activation of cytokine mediators, which activate the T-lymphocytes and HSP's as part of the adaptive immune response . Another immune response, which can occur, is the innate immune response . Innate immunity uses Natural Killer (NK) cells. Notably, the number of NK cells has been demonstrated to be proportional to lean muscle mass in the aged population. Thus it would seem that the maintenance of muscle mass would be extremely important insurance against morbidity. Progressive Resistance Training (PRT) has been proposed as an important anabolic stimulus to maintain muscle mass in people with sarcopenia . Importantly, sarcopenia commences in the 4th decade of life in sedentary people. The recommended dose of PRT has been 6-8 exercises of 40 minutes duration, at moderate intensity every 72 hours (see review by Krause 2003 for more detail). Evidence for the efficacy of this type of training comes from the literature on exercise for elderly people with sarcopenia as well as investigations into metabolic syndrome (syndrome X) whereby this stimulus intensity & duration is enough to improve insulin sensitivity in people with type II insulin resistant diabetes (Fig.6) Therefore, it is plausible that maintenance of muscle mass leaves a high concentration of NK cells ready for mobilisation by the innate immunity. Additionally, the metabolic responses of exercise maintain adaptive immune response HSP activity from being 'blunted' by inactivity.
Figure 6 : Progressive Resistance Training for 'fine-tuning' the immune system with exercise.
Treatment for chronic musculoskeletal dysfunction costs $US3.6 billion annually in Australia (fig 7). New and more effective treatment strategies have been advocated in NSW. These strategies have included using a more multi-modal treatment approach, greater use of cross referral between health professionals and the use of cognitive aspects of goal setting. NSW physiotherapists already use combinations of thorough verbal and physical assessment, manual therapy, muscle energy techniques, massage, dry needling (intra-muscular stimulation), yoga, Pilates, Feldenkreis, progressive relaxation, bio-feedback, etc, to be able to access both the physical and cognitive domains of neuro-immune responses.
Figure 7 The cost of mal-adaptive responses to trauma
Taken at face value, it seems counter-intuitive in that people must break down their bodies to enhance strength, endurance and power. Acute reactions to high volume - high intensity exercise is an immediate reduction in strength post exercise (up to 50-65% loss), followed by a short 'rebound', after which the strength decreases again for 24-48 hours. The first hour of recovery after exercise appears critical. If this physical stress is also accompanied by mental strain and/or emotional distress, the chances of illness or sports-related injuries increase. Both subjective measures of perceived stress and objective measures of stressful events were demonstrated to have a significant (9.2%) impact on recovery (Stults-Kohlemainen & Bartholomew 2012)
Central and Peripheral Fatigue and Central Motor Drive (CMD) as it relates to 'threat' to the CNS
Peripheral fatigue comprises changes in the metabolic milieu of the working muscles whereas central fatigue comprises of a failure by the central nervous system (CNS) to 'drive' the motor neurons, commonly referred to as a reduction in central motor drive (CMD). It is thought that the feedback from type III and type IV nerve receptors in muscles, about the peripheral metabolic milieu, is critical to CMD. However, in an interesting review, Markus Amann (2011, Med Sc Sp Ex, 43, 11, 2039-2045) argues that, when there is a direct threat to the CNS, as a result of adverse physiological circumstances, such as hypoglycaemia, mental stress/fatigue, or in the presence of extreme environmental influences, such as heat or severe hypoxia, these factors play a much greater influence than peripheral metabolic milieu. In the case of hypoxia, the exercising terminating threshold can be up to 30% less, where exhaustion becomes exercising limiting. Hence, when training at altitude, factors such as hypoxia and the other 'threats to the CNS' should be taken into consideration, epsecially when it comes to team training camps, where many influences out of the athletes control come into play.
Cognition and the neuro-immune response
Psychological factors such as 'over-reaching' at work or 'over training' at sport or cognitive mal-adaptation to dealing with pain can have a significant effect on which immune system is preferentially mobilised. Investigators have observed that defeated rats demonstrated decreased immune system sensitivity to glucocorticoid-mediated inhibition (Raison & Miller 2003). The development of glucocorticoid resistance correlated with a subordinate behavioural profile after defeat as well as correlating with the number of wounds received in fighting aggressive intruder mice. It was speculated that the risk of being wounded in hierarchical groups may have led to a condition for subordinated animals in which overall survival was favoured by promotion of rapid non-specific immunity, at the expense of more slowly developing specific immunity. Innate immunity is favoured by pro-inflammatory cytokines (esp TNF-alpha), which paradoxically can suppress specific (acquired) immune responses including T-cell proliferation and T-cell receptor signalling (Raison & Miller 2003), which presumably also includes HSP responses. Additionally, while mechanisms involving the immune system contribute to pain sensitivity, they also appear to be linked to basal nociceptive thresholds and are opioid dependent (Hutchinson et al 2004). Furthermore, gender differences suggest that high cytokine macrophage migration inhibiting factor (MIF) in younger males may have a protective effect on hippocampal neurones due to high testosterone levels. However, MIF was lower in people with pain in both sexes (Aloisi et al 2005) therefore suggesting increased vulnerability to hippocampal damage. This is significant because the hippocampus has important memory functions. Hence, the physiotherapist needs to be aware of how a perceived threat could potentially induce harmful non-context specific immune responses, which if chronically unmodulated can result in damage to the hippocampal neurones of the neuro-immune modulating system (fig 8). Therefore the physiotherapist may need to challenge the clients beliefs systems without being confrontational. Taken in the context of pain, work stressors and/or sporting endeavours, signals that activate and de-activate the cognitive behavioural response should be considered during the clinical reasoning process by setting realistic and achievable goals for the client, as well as using the past and current histories to ascertain the 'milestones' which have promoted or ameliorated chronic pain, disability and/or immune compromise
Figure 8 : Signals that influence the cognitive behavioural response
Notably, athletes who partake in heavy training schedules frequently complain of increased susceptibility to upper respiratory infections . After intense long-term exercise there is concomitant inflammation as well as a temporary suppression of the cellular immune response, 2-4 hours post exercise (Pedersen 1998). There is anecdotal evidence to suggest that endurance athletes may be more susceptible to certain cancers. The literature has described accomplished distance runners with Leukaemia. Lance Armstrong, multiple winner of the Tour de France is a well-known survivor of testicular cancer where there had been multiple metastases. In the early 1990's, over 10 young Scandanavian Orienteers suddenly died whilst resting such as in their sleep, at the starting line and at the breakfast table. Autopsies demonstrated massive cardiac scarring, which was considered to be due to tick bourn, viral and bacterial infections. Interestingly, these deaths appeared to be only associated with elite orienteers. However, some unexplained deaths in other Orienteers were noted but not followed up at the time. Therefore, it is important for athletes to enter their health status in their training diaries
Figure 9 : Muscle cellular immune response to post exercise trauma
Severe exercise (95%Vo2max ) increases Natural Killer (NK) count enhancing the cytotoxicity of NK to Naso-Pharyngeal Carcinoma (NPC). However, such exercise also promotes the platelet-impeded apoptosis of NPC induced by NK. Pre-treatment warm-up (60%Vo2max cycling for 20mins and 30mins recovery before severe exercise) increases the efficiency of the cytotoxicity of NK to NPC after severe exercise by reducing the extent to which platlets impede NK-NPC interaction while maintaining the increase in NK count and the cytotoxic granule protein contents induced by severe exercise. This is an important finding as it highlights an effective exercise regime for anti-tumor cytotoxicity (Wang et al 2008)
Fatigue, Overtraining and the Neuro-immune response
Exercise training to enhance performance requires that the athlete is loaded above their 'comfort zone' for performance enhancement and growth adaptation to occur. Fatigue induction is the first rule for endurance training adaptation. Paradoxically, fatigue is considered an initial alarm signal , which if ignored can lead to depletion of ATP at the actin-myosin cross bridge which initially induces cramps that eventually can lead to tetanic muscle contraction and potentially death. Significantly ATP has both pro as well as anti-inflammatory properties . (fig 4). The major metabolic adaptations to training occur within the skeletal muscles, liver and kidneys' (Petibois et al 2002). In addition to metabolic stress, the muscle receives mechanical stress. Together, the disruption of cellular architectural proteins and chemical aggregation on subcellular contents produce highly reactive oxygen species (ROS). An imbalance between ROS actions and anti-oxidant defence capacity of the muscle cells has been implicated in over-training. Additionally, glutamine responses have been shown to augment during exercise and fall significantly for several hours post exercise. This is significant, as glutamine constitutes the metabolic link between active skeletal muscles and the capacity of the immune system . However, researchers have found conflicting evidence against this latter hypothesis (Petibois et al 2002). Another mediator of immune response may be leptin, which is released from adipocytes (fat) and seems to affect the feedback mechanism of the hypothalamic-pituitary-gonadal axis (HPGA) . Global levels of serum leptin have been shown to decrease in highly trained endurance athletes. However, little data exists to verify any correlation with fat mass and over-training in endurance athletes (Petibois et al 2002). Energy status of athletes seems to be critical as the ability of an endurance athlete to train is carbohydrate-lipid metabolism dependent rather than protein metabolism dependent. Sparing of protein is not only fortuitous to the mechanical contractile element but may also be immune-sparing (fig 1). Unfortunately, due to the complexity of hormonal interactions, multiple subsystems and redundancy, the examination of testosterone : cortisol ratio's alone have not been shown to be a significant marker for over-training (Petibois et al 2002). Alterations in nocturnal catecholamine secretion and reduced cortisol concentrations have also been implicated in over-training. Reduced cortisol synthesis is thought to reduce the modulation of sympathetic tone, potentially leading to enhanced catecholamine facilitation of memory formation and subsequent avoidance of potentially hostile environments (Raison & Millier 2003). Therefore, it is interesting to speculate that training to fatigue requires specific 'on-off signals' such as performance goals and recuperation strategies, as well as adequate provision of energy substrates to meet the metabolic demands of exercise training. Hereby, performance enhancement and growth adaptation can occur whilst avoiding over-training by positively mobilising the immune system with a finely tuned training regime, which makes sense to the athlete.
The subjective examination to screen for symptoms of over-training
Since biological markers of over-training show conflicting results it may be more useful for the athlete and trainer and physiotherapist to use psychological markers of over-training. These include feelings of depression, general apathy, decreased self esteem, emotional instability, difficulty in concentrating, sensitivity to environmental and emotional stress, fear of competition, changes in personality, decreased ability to narrow concentration, increased internal and external distractibility, decreased capacity to deal with large amounts of information, and giving up when the going gets tough (Smith 2000). Immunological markers include increased susceptibility to and severity of illnesses, colds and allergies, flu-like illness, unconfirmed glandular fever, minor scratches healing slowly, swelling of lymph glands, and one-day colds (Smith 2000). Therefore, it is important to use a training diary to monitor these signs & symptoms, as a well-structured training programme can be beneficial to the immune system, yet over-training can be detrimental and in some instances fatal (e.g. rhabdomyolysis (see website : www.members.tripod.com/~baggas/rhabdo.html )
General Adaptation Syndrome (GAS) and Allostasis
Selye (1936) recognized and defined 3 stages of a general adaptation syndrome (GAS): alarm, resistance, and exhaustion . The first two phases were considered adaptive, whereas the final stage represented the breakdown of adaptive capacity. Therefore, paradoxically, the physiological systems activated by stress can not only protect and restore but also damage the body (McEwen 1998). The ability to achieve stability through change has been called allostasis, and is considered critical to survival. Through allostasis, the autonomic nervous system, the hypothalamic-pituitary-adrenal (HPA) axis, and the cardiovascular, metabolic, and immune systems protect the body by responding to internal and external stress. The stress from the wear and tear that results from chronic over/underactivity of allostasis is referred to as allostatic load (McEwen 1998). How a person perceives a stimuli (conscious or subconscious) and whether a person perceives it as a threat (psychological or physical) is crucial in determining behavioural (fright-fight-flight) and physiological (calmness or palpitations, altered cortisol) responses (fig 9). Obviously, in either scenario the person's physical health will determine the ability to mount these responses. The most common allostatic response involves the sympathetic nervous system (SNS) and the HPA axis, which release catecholamines from the nerves and adrenal medulla as well as the secretion of corticotropin from the pituitary gland. Corticotropin in turn modulates that release of cortisol from the adrenal cortex.
Figure 10: Signal perception and the allostatic response
McEwen (1998) descibed four situations for allostatic loads
- Frequent stress
- Lack of time for adaptation to repeated stress eg frequent public speaking
- Inability to shut off an allostatic response after a stress has terminated. Intense athletic training also induces allostatic load with elevated SNS and HPA axis activity, which results in the mobilisation of fat, weight loss, dysmenorrhea &/or amenorrhea (HPGA axis – Follical Stimulating Hormone {FSH}, Luteinising Hormone {LH} and Opioid balance), and the often, related condition of anorexia nervosa (Boyar et al 1977, Loucks et al 1989 in McEwen 1998). According to the “glucocorticoidcascade hypothesis” wear and tear on the hippocampus due to HPA over-activation can result in cognitive impairment (declarative and spatial memory) as demonstrated in rats (Sapolsky 1992, 1986; Seeman et al 1994, 1997; Meaney et al 1988; Lupien et al 1994 in McEwen 1998). Furthermore, suppression of the HPGA axis by increased opioid levels leads to hypogonadism, which causes changes in sexual interest and function, depression, as well as muscle wasting and osteoporosis (Aloisi et al 2005).
- Notably, inadequate response by some allostatic mechanisms results in compensatory increases in other mechanisms. For example inadequate secretion of cortisol results in reduced counter-regulation of inflammatory cytokines.
Figure 11: Allostatic load response
In humans HPA hypo-responsiveness has included people suffering with fibromyalgia, chronic fatigue syndrome and children with atopic dermatitis (McEwen 1998) as well as individuals with failed disc surgery (Geiss et al 2005). Furthermore, in post-traumatic stress disorder basal HPA activity may be low, however the reactivity to stress may not be blunted (McEwen 1998). Figures 12 & 13 list behavioural and clinical evidence for altered allostasis which can perpetuate chronic musculoskeletal dysfunction.
Figure 12: Clinically significant behavioural evidence for altered allostasis
Figure 13: Clinical physiological evidence for neuro-immune involvement in altered allostasis
Anticipatory anxiety can drive the secretion of mediators like corticotropin, cortisol and adrenalin and for these reasons prolonged anxiety is also likely to lead to allostatic load. Unfortunately, the previously discussed impairment of the hippocampus decreases the reliability and accuracy of contextual memories. Therefore, this may influence allostatic responses by preventing pre-emptive cortical processing of the information needed to evaluate the nature of the threat (Sapolsky 1990 in McEwen 1998). Importantly, the hippocampus would normally regulate the stress response by modulating the HPA axis (Jakobson & Sapolsky 1991 in McEwen 1998). For example, in a sport such as orienteering, well-trained athletes regulate allostatic load through anticipation of the upcoming terrain through visualisation of successful prior experiences in similar terrain prior to the race, as well as accurate map reading for recognition and hence prediction of upcoming terrain during the race. Similarly, the clinician can aid the client in their rehabilitation by setting realistic goals , thereby fine-tuning their anticipatory and hence perceptive and predictive responses (see Krause 2002 ).
Although speculative, it would seem logical that periodisation of training may be a useful tool in fine-tuning allostatic responses. Indeed, periodisation and varied training have been used by coaches to reduce the risk of over-training, as well as enhance efficiency through more qualitative rather than quantitative training.
Periodisation of endurance and plyometric training (Krause 2003)
Hence what Selye (1936) recognized and defined 3 stages as a general adaptation syndrome (GAS) of alarm, resistance, and exhaustion can be used by the clinician in recognizing whether the client is in the first two adaptive phases, or whether they are in the final stage which represents the breakdown of adaptive capacity. Furthermore, the clinician cognizant with these adaptive strategies can reduce the risk of entering the final stage by adequate planning (e.g. periodisation), goal setting and preparatory education, thereby reducing anticipatory anxiety.
Figure 14: are the Kubler-Ross stages of dying similar to those of musculoskeletal disability?
Cognitive Behavioural Therapy
By using a Cognitive Behavioural Therapy (CBT) approach, physiotherapists could potentially gain yet another powerful assessment and treatment tool in their arsenal of multi-modal assessment and treatment approaches for people trying to manage pain, immune responses and musculoskeletal dysfunction. In this manner CBT is used to assess, monitor and change central nervous system (CNS), peripheral nervous system (PNS) and immune processing of various stressors. As discussed previously the peripheral sympathetic nervous system (pSNS) interacts with the central nervous system as well as the hypothalamic-pituitary-adrenal axis for the modulation of inflammation and immune responses. The Superior Cervical Ganglion (SCG) and DRG of th pSNS have multiple alpha 2 – adrenergic receptor subtypes, which are functionally active in response to nerve injury, inflammation or physiological and patho-physiological conditions (Gold et al 1997). Hence, concomitant injury to the peripheral sympathetic ganglia (e.g. after whiplash injury to the SCG), may not only compromise the regulation of blood flow to the DRG (Haebler et al 2000) but also reduce the modulation of inflammation and neuro-immune responses at the sites of peripheral nerve terminals (see Krause 1997 ). Therefore, with a compromised peripheral nervous system and altered central nervous system processing, it would seem wise to follow a CBT approach to treatment, whereby higher centre signal processing can be modulated through behavioural and perceptional changes to peripheral signalling stimuli. However, in chronic neuro-immune stress states we know that hippocampal damage may affect memory, which in turn can affect anticipatory anxiety which can enhance negativity in perception. Since the conscious brain can only process one piece of information at a time and can only hold 6 pieces of information in short term memory, it becomes imperative to access the subconscious because the majority of information processing occurs here ( Krause 2002 ). Imagery, meditation, and verbalisation strategies can be used to access the subconscious and favourably alter negative perceptive states (fig 15).

Figure 15: Cognitive behavioural therapy and exercise
A B C D
Socratic Questioning - the use of provocative questioning to overcome peoples underlying assumptions and beliefs
- What are the facts abd what are my subjective perceptions?
- What is the evidence which supports my perceptions?
- What is the evidence which contradicts my perceptions?
- Are there thinking errors?
- How else can the situation be perceived?
Behavioural Disputing - while behaviours can reinforce unhelpful cognitions, they can be used to dispute them. Behaving in a way that is inconsistent with certain cognitions can help us discover that those cognitions are incorrect.
Goal Directed Thinking - involves focussing on the self-defeating nature of our cognitions, recognising that our current perceptions prevent us from achieving the things we want. In goal-directed thinking we remind ourselves to remain focused on our goals.
Overcoming Low Frustration Tolerance (LTF) - overcoming the use of 'shoulds', 'black & white' thinking, catastrophising, use of extremes "always" can occur by using the
Antecedents Beliefs Consequences & Disputes (ABCD)
Examine
-
the situation which triggers the response
-
the cognitions about the situation
-
the way that we feel and behave
-
disputing the belief
CBT employs cognitive and meta-cognitive process by examining the
-
situation
-
feelings
-
thoughts
-
beliefs
-
thinking errors
Instituting a
-
disputing strategy
through
-
positive actions
This methodology can be used to improve mental, emotional and physical well-being.
Several lines of evidence suggest that treatment using the psycho-cognitive domain to evaluate perception can substantially influence treatment outcome. It would appear that fear-avoidance and distress are important factors in the development of pain-related disability (Boersma & Linton 2005). Clients with higher treatment expectancy demonstrated better pain coping and control, active and positive interpretation of pain, and less disability compensation. Additionally, these positive perception attributes significantly predicted post CBT outcome measures in people suffering chronic pain (Goossens et al 2005). Perception has been demonstrated to be positively influenced by educational sessions where fear reductions significantly decreased pain intensity through graded exposure and this remained up to 6 months post intervention (de Jong et al 2005). Psychometric evaluation strategies such as the Chronic Pain Coping Inventory (CPCI) provides clinicians with a measure of the frequency with which patients use coping strategies, which are both encouraged (exercise/stretching, relaxation, task persistence) and discouraged (guarding, resting, asking for assistance) (Jensen et al 1995). Therefore, adherence to positive coping strategies may be evaluated and correlated with any changes to perception traits such as reduction in 'fear-avoidance' behaviour
Severe acute or chronic infection and/or inflammation may result in muscle atrophy due to the protein mobilisation during the immune response. This could compromise both the metabolic and mechanical loading capacity of the muscles. Therefore depending upon the degree and extent of cachexia the body may take months if not years to recover. Hence, in such extreme cases, it would seem appropriate to set long and short term goals, which are realistic and attainable in the quest to maintain and/or re-establish allostasis. Clinically, an activity pacing scale has been used in people suffering with fibromyalgia (Nielson et al 2001). This could be used for people to monitor their allostatic load, and together with assessing for the symptoms of 'over-training' an indication of allostasis may be obtained. Although, highly speculative these ideas seem very plausible and may be a means to harness the healing potential of the neuro-immune system.
Evaluation of the outcomes of CBT programmes has been described as 'difficult'. A recent literature review concluded no significant differences between behavioural treatment and exercise therapy (Ostelo et al 2004). "Frequently the treatment effect size is modest and the specificity of one treatment approach over another hasn't been validated because little is known about the biobehavioural mechanisms leading to chronic pain and disability." As such, it was concluded that client characteristics needed to be matched to treatment programs (Vlayaen & Morley 2005). By using a CBT approach, physiotherapists could potentially gain yet another powerful assessment and treatment tool in their arsenal of multi-modal assessment and treatment approaches for people trying to manage pain and musculoskeletal dysfunction. In this manner CBT can be used to assess, monitor and change CNS, PNS and immune processing of various stressors.
Conclusion
Nutritional advice together with a cognitive behavioural approach to exercise therapy has been advocated to harness the positive mechanical, metabolic and immune effects of enhanced muscle mass which should improve allostasis. This approach can be used for training athletes. Using a structured training program involving periodisation and goal setting the person should be able to enhance their performance as well as 'fine-tune' their immune system's allostatic loading capacity. Additionally, enhanced muscle mass provides a rich source of protein for both the adaptive and innate immune systems. When used in a chronic disability setting, maintenance of a structured clinical reasoning process which engages the client by educating them on the aims and objectives and in particular the outcomes (feedback) of the treatment management strategy can reduce allostatic load. Hereby, all the tools the physiotherapist has at their disposal can be integrated purposefully, without falling into the trap that 'more is better' (fig 16). Eventually, independence and the adoption of a self-management approach to monitoring chronic disability can be attained by the client. This latter aspect is particularly important, as there are potentially many clinicians who make a living creating client dependency. As Australian physiotherapists begin to adopt a CBT strategy to their already multi-modal evidence based approach it will be interesting to evaluate it's future affect on the $AUD4.7 billion annual cost (The Australian Financial Review: Friday 10 June 2005 p9) of musculoskeletal disability. Taken together, performance enhancement without compromising but rather enhancing the immune system should be the ultimate goal of exercise training.
Figure 16: Multi-factorial and multi-modal physiotherapeutic intervention model
Presentation in Rome : 7-9 October 2005
Millar et al (Clin Orthop Relat Research, 2008, May 6) used a running rat model induced suprapsinatus tendonopathy to demonstrate the release of heat shock proteins. Additionally, the up-regulation of HSP was further demonstrated on patients undergoing arthroscopic stabilisation sugery (n=10). They concluded that these findinggs suggest that HSP play a role in the cascade of stress-activated programmed cell death and degeneration in tendonopathy.
Reduced reactivity and enhanced negative feedback sensitivity of the hypothalamus–pituitary–adrenal axis in chronic whiplash-associated disorder
Pain, Volume 119, Issues 1-3, 15 December 2005, Pages 219-224
Jens Gaab, Susanne Baumann, Angela Budnoik, Hanspeter Gmünder, Nina Hottinger, Ulrike Ehlert
Abstract
Dysregulations of the hypothalamus–pituitary–adrenal (HPA) axis have been discussed as a physiological substrate of chronic pain and fatigue. The aim of the study was to investigate possible dysregulations of the HPA axis in chronic whiplash-associated disorder (WAD). In 20 patients with chronic WAD and 20 healthy controls, awakening cortisol responses as well as a short circadian free cortisol profile were assessed before and after administration of 0.5 mg dexamethasone. In comparison to the controls, chronic WAD patients had attenuated cortisol responses to awakening, normal cortisol levels during the day, and showed enhanced and prolonged suppression of cortisol after the administration of 0.5 mg dexamethasone. Dysregulations of the HPA axis in terms of reduced reactivity and enhanced negative feedback suppression exist in chronic WAD. The observed endocrine abnormalities could serve as a systemic mechanism of symptoms experienced by chronic WAD patients.
Systemic Immune Response in Whiplash Injury and Ankle Sprain: Elevated IL-6 and IL-10. Clinical Immunology, Volume 101, Issue 1, October 2001, Pages 106-112
Jouko Kivioja, Volkan Özenci, Luciano Rinaldi, Mathilde Kouwenhoven, Urban Lindgren, Hans Link
Abstract
Whiplash injury and whiplash-associated disorders (WAD) are significant problems of modern society. Numerous attempts have been made to characterize the nature of whiplash injury. Whether the immune system is involved during the disease process is not known. In a prospective study, using enzyme-linked immunospot (ELISPOT) assays, we examined numbers of blood mononuclear cells (MNC) secreting pro- (IFN-?, TNF-a, IL-6) and anti-inflammatory (IL-10) cytokines in patients with WAD and, for reference, patients with ankle sprain and multiple sclerosis and healthy subjects. An immune response reflected by elevated numbers of TNF-a- and IL-10-secreting blood MNC was observed in patients with WAD examined within 3 days compared to 14 days after the whiplash injury. The patients with WAD examined within 3 days after the injury had also higher numbers of IL-6 and IL-10 secreting blood MNC compared to healthy subjects. The alterations of cytokine profiles observed in WAD were also observed in patients with ankle sprain when examined within 3 days after trauma. In contrast, there were no differences for cytokine profiles between patients with WAD examined 14 days after the whiplash injury and healthy subjects. Relatively minor trauma like WAD and ankle sprain are associated with a systemic dysregulation in numbers of cells secreting pro- as well as anti-inflammatory cytokines.
References for Neurohormonal musculoskeletal injuries
Aloisi AM, Pari G, Ceccarelli I, Vecchi I, Ietta F, Lod L, Paulesu L (2005). Gender-related effects of chronic non-malignant pain and opioid therapy on plasma levels of macrophage migration inhibitory factor (MIF). Pain, 115, 142 to 151
Apkarian AV, Sosa Y, Krauss BR, Thomas PS, Fredrickson BE, Levy RE, Harden RN, Chialvo DR (2004) Chronic pain patients are impaired on an emotional decision-making task. Pain, 108, 129 to 136.
Bergman S, Jacobsson LTH, Herrstroem P, Petersson IF (2004). Health status as measured by SF-36 reflects changes and predicts outcome in chronic musculoskeletal pain: a 3-year follow up study in the general population. Pain, 108, 115 to 123
Boersma K, Linton SJ (2005). Screening to identify patients at risk: profiles of psychological risk factors for early intervention. Clinical Journal of Pain, 21, 1, 38 to43
Chazaud B, Brigitte M, Yacoub-Youssef H, Arnold L, Gherardi R, Sonnet C, Lafuste P, Chretien F (2009). Dual and Beneficial Roles of Macrophages During Skeletal Muscle Regeneration. Exercise and Sports Science Reviews, 37, 1, 18 to 22
De Jong JR, Vlaeyen JW, Onghena P, Goossens ME, Geilen M, Mulder H (2005). Fear of movement/(re)injury in chronic low back pain: education or exposure in vivo as mediator to fear reduction. Clin J Pain, 21, 1, 9 to 17
De Leo JA, Yezierski RP (2001) The role of neuroinflammation and neuroimmune activation in persistent pain. Pain, 90, 1 to 6
Lieber RL, Fridén J (2002). Mechanisms of muscle injury gleaned from animal models. American Journal of Physical Medicine and Rehabilitation, 81, 11, S70 to S79
Geiss A, Rohleder N, Kirschbuam C, Steinbach K, Bauer HW, Anton F (2005). Predicting the failure of disc surgery by a hypofunctional HPA axis: evidence from a prospective study on patients undergoing disc surgery. Pain, 114, 104 to 117
Gold MS, Dastmalchi S, Levine JD (1997) Alpha 2 – adrenergic receptor subtypes in rat dorsal root and superior cervical ganglion neurons. Pain, 69, 179 to 190.
Goossens ME, Vlaeyen JW, Hidding A, Kole-Snijders A, Evers SM (2005). Treatment expectancy affects the outcome of cognitive behavioural interventions in chronic pain. Clin J Pain, 21, 1, 18 to 26
Grotle M, Vollestad NK, Veierod MB, Brox JI (2004). Fear-avoidance beliefs and distress in relation to disability in acute and chronic low back pain. Pain, 112, 343 to 352
Haebler H-J, Eschenfelder S, Liu X-G, Jaenig W (2000). Sympathetic-sensory coupling after L5 spinal nerve lesion in the rat and its relation to changes in dorsal root ganglion blood flow. Pain, 87, 335 to 345
Hamilton A (2005) How much protein do athletes need – and how safe are high protein diets? Peak Performance, 208, 1 to 4
Hasko G (2001) Receptor mediated interaction between the sympathetic nervous system and immune system in inflammation. Neurochemical Research, 26, 8/9, 1039 to 1046
Hocheisel U, Unger T, Mense S (2005). Excitatory and modulatory effects of inflammatory cytokines and neurotrophins on mechanosensitive group IV muscle afferents in the rat. Pain, 114, 168 to 176
Hutchinson R, La Vincente SF, Somogyi A (2004). In vitro opioid induced proliferation of peripheral blood immune cells correlates with in vivo cold pressor pain tolerance in humans: a biological marker of pain tolerance. Pain, 110, 751 to 755.
Imbe H, Murakami S, Okamoto K, Iwai-Liao Y, Senba E (2004) The effects of acute and chronic restraint stress on activation of ERK in the rostral ventromedial medulla and locus coereleus. Pain, 112, 361 to 371
Jensen MP, Turner JA, Romano JM, Strom SE (1995) The chronic pain coping inventory: development and preliminary validation. Pain, 60, 203 to 216
Keast D (1996). Immune responses to overtraining and fatigue. In: Exercise and Immune Function Hoffman-Goetz (Ed). Boca Raton, FL: CRC Press, pp 121 to 141
Kovanen V (2002). Intramuscular extracellular matrix: complex environment of muscle cells. Exerc. Sport Sci. Rev, 30, 1, 20 to25
Liddle SD, Baxter GD, Gracey JH (2004). Exercise and chronic low back pain: what works? Pain (2004), 107, 176 to 190
Lieber RL, Shah S, Friden J (2002). Cytoskeletal disruption after eccentric contraction induced muscle injury. Clinical orthopaedics and related research, 403S, S90-S99
Marks DB, Marks AD, Smith CM (1996). Inter-tissue relationships in the metabolism of amino acids. In: Basic Medical Biochemistry (1 st ed). Baltimore: Williams and Wilkins, pp 647 to 666
McCall GE, Gosselink KL, Bigbee AJ, Roy RR, Grindeland RE and Edgerton VR (2001) Muscle afferent-pituitary axis: A novel pathway for modulating the secretion of pituitary growth factor. Exercise and Sports Sciences Reviews, 29, 4, 164 to 169
McEwen BS (1998) Protective and damaging effects of stress mediators. The New England Journal of Medicine, 338, 3, 171 to 179
Mosely, PL (2000) Exercise, Stress, and the Immune Conversation. Exercise and Sports Sciences Reviews, 28, 3, 128 to 132
Nielson WR, Jensen MP, Hill ML (2001) An activity pacing scale for chronic pain coping inventory: development in a sample of patients with fibromyalgia syndrome. Pain, 89, 111 to 115
Ostelo RW, van Tulder MW, Vlaeyen JW, Linton SJ, Morley SJ, Assendelft WJ (2004) Behavioural treatment for chronic low-back pain. Cochrane Database Syst Rev. 2005 Jan 25;(1):CD002014
Pedersen BK, Rohde T, Ostrowski K (1998) Recovery of the immune system after exercise. Acta Physiologica Scandinavia, 162, 3, 325 to 332
Petibois C, Cazorla G, Poortmans J-R, Deleris G (2002). Biochemical aspects of overtraining in endurance sports : a review. Sports Medicine, 32, 13, 867 to 878
Raison CL, Miller AH (2003) When not enough is too much: the role of insufficient glucocorticoid signalling in the pathophysiology of stress-related disorders. The American Journal of Psychiatry, 160, 9, 1554 to 1565
Ramer MS, Murphy PG, Richardson PM, Bisby MA (1998) Spinal nerve lesion-induced mechanoallodynia and adrenergic sprouting in sensory ganglia are attenuated in interleukin-6 knockout mice. Pain, 78, 115 to 121
Sedan O, Sprecher E, Yarnitsky D (2005) Vagal stomach afferents inhibit somatic pain perception. Pain, 113, 354-359
Smith LL (2000) Cytokine hypothesis of overtraining: a physiological adaptation to excessive stress. Med. Sci. Sports Ex, 32, 2, 317 to 331
Sterling M, Jull G, Vicenzino B, Kenardy J, Darnell R (2005) Physical and Psychological factors predicting outcome following whiplash injury. Pain, 114, 141 to 148
Stults-Kolehmainen MA, Bartholomew JB (2012) Psychological stress impairs short-term muscular recovery from resistance exercise. Med Sc Sp Ex, 44, 11, 2220-2227
Sullivan MJL, Lynch ME, Clark AJ (2005) Dimensions of catastrophic thinking associated with pain experience and disability in patients with neuropathic pain conditions. Pain, 113, 310 to 315
Vlaeyen JW, Morley S (2005). Cognitive-behavioural treatments for chronic pain: what works for whom? Clin J Pain, 21, 1, 1 to 8
Wagenmakers JM (1998). Muscle amino acid metabolism at rest and during exercise: role in human physiology and metabolism. Exercise and Sports Science Reviews Holloszy JO (Ed). Baltimore : Williams and Wilkins, 1998, pp 287 to 314
Wang J-S, Chung Y, Chow S-E (2008). Exercise affects platelet-impeded antitumor cytotoxicity of natural killer cell. Medicine & Science in Sports & Exercise, 41, 1, 115 to122
Watkins LR Maier SF (2000). The pain of being sick: implications of immune-to-brain communication for understanding pain. Annu. Rev. Psychol. 51, 29 to 57
Williams KA, Petronis J, Smith D, Goodrich D, Wu J, Ravi N, Doyle EJ, Juckett G, Kolar MM, Gross R, Steinberg L (2005). Effect of Iyengar yoga therapy for chronic low back pain. Pain, 115, 107 to 117
Last update : 29 October 2017