Benign Paroxysmal Positional Vertigo (BPPV)
Back in Business Physiotherapy
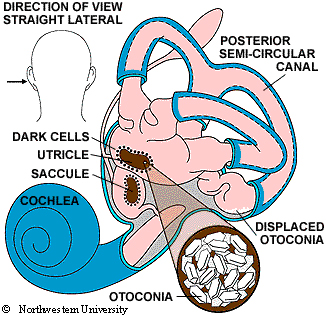
Benign Paroxysmal Positional Vertigo (BPPV) dizziness is thought to be due to the collection of small crystals in the inner ear.
BPPV is a common cause of dizziness. About 20% of all dizziness is due to BPPV. The older you are, the more likely it is that your dizziness is due to BPPV, as about 50% of all dizziness in older people is due to BPPV. In a recent study, 9% of a group of urban dwelling elders were found to have undiagnosed BPPV (Oghalai, J. S., et al., 2000).
Symptoms
The symptoms of BPPV include dizziness or vertigo, light headedness, imbalance, and nausea. Activities which bring on symptoms will vary among persons, but symptoms are almost always precipitated by a change of position of the head with respect to gravity. Getting out of bed or rolling over in bed are common "problem" motions. Because people with BPPV often feel dizzy and unsteady when they tip their heads back to look up, sometimes BPPV is called "top shelf vertigo." Women with BPPV may find that the use of shampoo bowls in beauty parlours brings on symptoms. An intermittent pattern is common. BPPV may be present for a few weeks, then stop, then return.
Causes
The most common cause of BPPV in people under age 50 is head injury . There is also an association with migraine (Ishiyama et al, 2000). In older people, the most common cause is degeneration of the vestibular system of the inner ear. BPPV becomes much more common with advancing age (Froeling et al, 1991). In half of all cases, BPPV is called "idiopathic," which means it occurs for no known reason. Viruses affecting the ear such as those causing vestibular neuritis , minor strokes such as those involving anterior inferior cerebellar artery (AICA) syndrome", and Meniere's disease are significant but unusual causes. Occasionally BPPV follows surgery, where the cause is felt to be a combination of a prolonged period of supine positioning, or ear trauma when the surgery is to the inner ear (Atacan et al 2001).
Treatment
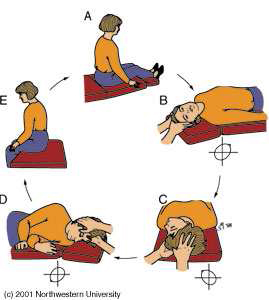
The Epley maneuver is also called the particle repositioning, canalith repositioning procedure, and modified liberatory maneuver. It involves sequential movement of the head into four positions, staying in each position for roughly 30-120 seconds. The recurrence rate for BPPV after these maneuvers is about 30 percent at one year, and in some instances a second treatment may be necessary. After either of these maneuvers, you should be prepared to follow the instructions below, which are aimed at reducing the chance that debris might fall back into the sensitive back part of the ear. According to Herdman et al (1993) the cure rate is 80%
Post-Maneuver Management
1. Wait for 10 minutes after the maneuver is performed before going home. This is to avoid "quick spins," or brief bursts of vertigo as debris repositions itself immediately after the maneuver. Don't drive yourself home.
2. Sleep semi-recumbent for the next two nights. This means sleep with your head halfway between being flat and upright (a 45 degree angle). This is most easily done by using a recliner chair or by using pillows arranged on a couch (see figure 3). During the day, try to keep your head vertical. You must not go to the hairdresser or dentist. No exercise which requires head movement. When men shave under their chins, they should bend their bodies forward in order to keep their head vertical. If eye drops are required, try to put them in without tilting the head back. Shampoo only under the shower.
3. For at least one week, avoid provoking head positions that might bring BPPV on again.
- Use two pillows when you sleep.
- Avoid sleeping on the "bad" side.
- Don't turn your head far up or far down.
Be careful to avoid head-extended position, in which you are lying on your back, especially with your head turned towards the affected side. This means be cautious at the beauty parlour, dentist's office, and while undergoing minor surgery. Try to stay as upright as possible. Exercises for low-back pain should be stopped for a week. No "sit-ups" should be done for at least one week and no "crawl" swimming. (Breast stroke is OK.) Also avoid far head-forward positions such as might occur in certain exercises (i.e. touching the toes). Do not start doing the Brandt-Daroff exercises immediately or 2 days after the Epley or Semont maneuver, unless specifically instructed otherwise by your health care provider.
4. At one week after treatment, put yourself in the position that usually makes you dizzy. Position yourself cautiously and under conditions in which you can't fall or hurt yourself. Let your doctor know how you did.
www.back-in-business-physiotherapy.com
Atacan E, Sennaroglu L, Genc A, Kaya S. Benign paroxysmal positional vertigo after stapedectomy. Laryngoscope 2001;111: 1257-9. Froehling DA, Silverstein MD, Mohr DN, Beatty CW, Offord KP, Ballard DJ. Benign positional vertigo: incidence and prognosis in a population-based study in Olmsted County, Minnesota. Mayo Clin Proc 1991 Jun;66(6):596-601.
Herdman SJ, et al. Single treatment approaches to benign paroxysmal positional vertigo. AOHNS 1993 Apr;119(4):450-454. Oghalai, J. S., et al. (2000). "Unrecognized benign paroxysmal positional vertigo in elderly patients." Otolaryngol Head Neck Surg (AOHNS) 122(5): 630-4.

























































































































