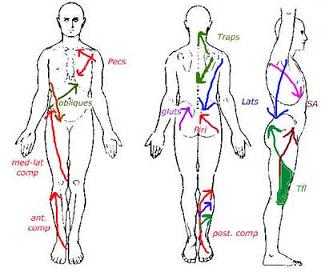
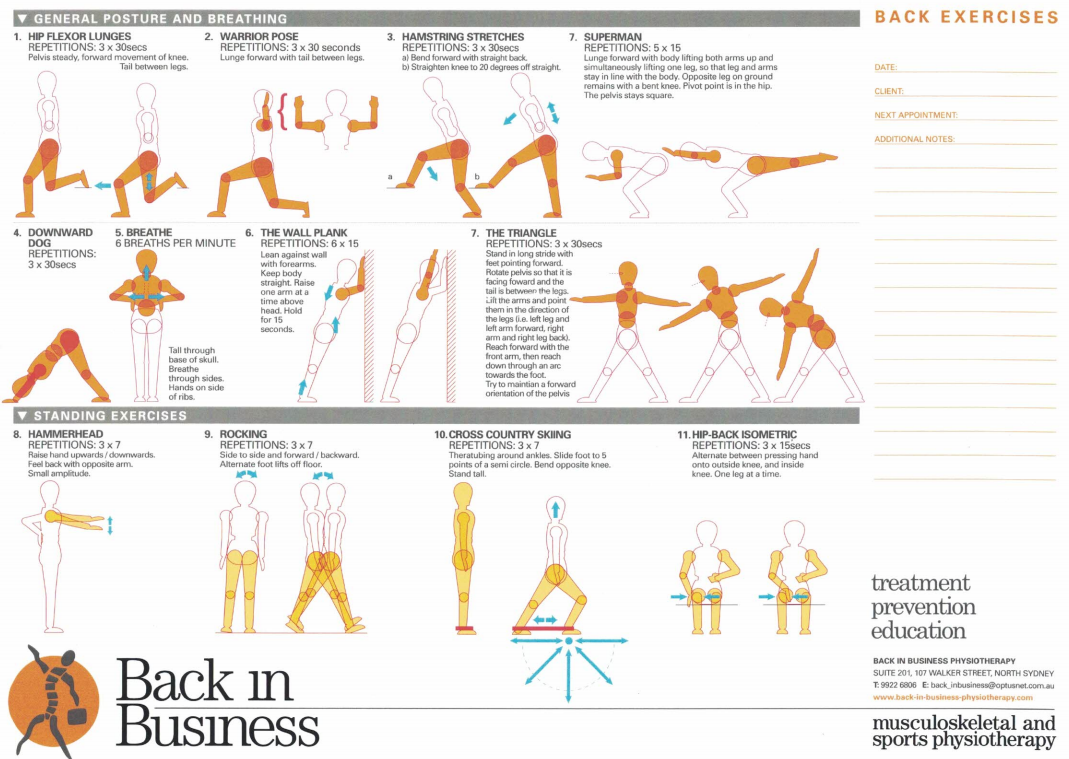
At Back in Business Physiotherapy we treat low back pain using a multi-modal approach to assessment and treatment. Frequently, the low back is 'the meat in the sandwich' where pelvic and hip dysfunction, combined with thoracic hypo/hypermobility result in adverse biomechanical loading of the lumbar spine. The spine and pelvis need to be considered as lying in a sling of muscles extending from the front, back and sides of the legs over the abdominal cavity and lumbar spine up to the rib cage. As such treating the joints in these regions with mobilsations, the soft tissue with massage and fascial releases and the muscles with muscle energy techniques, exercises and dry needling create a whole body, multi-modal, multi-dimensional approach to our treatments.
|
Low back pain can cause and can be caused through the interaction of multiple sites of dysfunction.
"the last straw to break the camels back" may be caused by 'overuse, abuse, misuse and disuse'
The physiotherapist needs to apply clinical reasoning to ascertain the "cause of the cause" so that treatment is meaningful and time effect. |
|
|
|
|
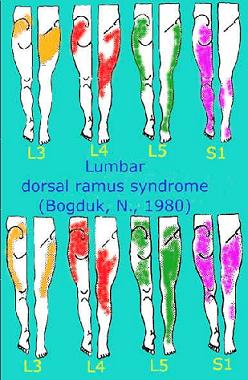
| This example demonstrates the frequent referral of 'somatic pain' into the limbs.
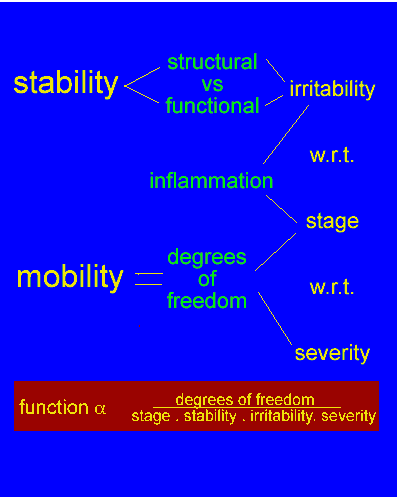
Central neurophysiological mechanisms suggest a role for the physiotherapist in identifying the source of symptoms. Additionally, the physiotherapist is required to make realistic prognosis based on the 'stage, severity, stability, and irritability' of the dysfunction' |
|
Connell AT (2008) Concepts for assessment and treatment of anterior knee pain related to altered spinal and pelvic biomechnics: a case report. Manual Therapy, 13, 560-563 This author used 3 sessions of treatment to the T10/11, T11/12, T12/L1 and L5/S1 to improve the ROM and ability to squat in a patient with anterior knee pain. Grindstaff TL et al (2009) Effects of lumbopelvic joint manipulation on quadriceps activation and strength in healthy individuals. Manual Therapy, 14, 415-420. These investigators found a significant increase in the ability to produce quadriceps force (+3%) and activation (+5%) immediatley following lumbopelvic joint manipulation
Green A and Perry (2008) An investigation into the effects of a unilaterally applied lumbar mobilisation technique on peripheral sympathetic nervous system activity in the lower limbs. Manual Therapy, 13, 492-499. These investigators examined 45 healthy naive males and performed a unilateral Posteroanterior technique to the zygopophyseal joint of L4/5 and recorded skin conductance in the lower limb using a randomized control trial. They found mobilsations at 2Hz resulted in side-specific peripheral SNS changes in the lower limbs. In their review they suggested that it is the oscillatory component of the mobilisation which has the greatest effect on the SNS (Gebber et al 1999, Kenny et al 1991, McGuiness et al 1997). The effect reported was 13.5% (+/- 20.25). Proposed mechanisms were direct stimulation of the SNS ganglion, soft tissue joint receptor reflexes, myogenic reflexes and descending modulatory responses. Bialosky JE et al (2009) The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Manual Therapy, 14, 531-538. Their review concluded that the result of a mechanical input from joint mobilisations produced a cascade of peripheral and central nervous system responses which provide an explanation for immediated and lasting clinical outcome. van Vliet PM & Heneghan (2006) Motor control and the management of musculoskeletal dysfunction. Manual Therapy, 11, 208-213. Feedforward mechanisms, an essential element to motor control, are altered in neurologically intact patients with chronic neck and low back pain can be the result of cortical neuroplasticity. Wallwork TL et al (2009) The effect of chronic low back pain on size and contraction of the lumbar multifidus muscle. Manual Therapy, 14, 496-500. Results showed a significantly smaller cross sectional area of the multifidus muscle for the subjects with CLBP as well as reduced percent thickness contraction. Green A & Dolan KJ (2006). Lumbar spine reposition sense: the effect of a 'slouched' posture. Following 300secs of slouch the lumbar spine demonstrated a reduced ability to reposition sense. An increase in reposition error by more than 2.35degrees and less than 5.48degrees was found. O'Sullivan et al (2006). The relationship between posture and back endurance in industrial workers with flexion-related low back pain. LBP subjects had significantly reduced back muscle endurance. LBP subjects sat with less hip flexion suggesting increased posterior pelvic tilt in sitting. LBP subjects postured their spines significantly closer to their end of range lumbar flexion in 'usual sitting' than healthy controls. Hodges P & Gandevia SC (2000) Activation of the human diaphragm during repetitive postural task. Journal of Physiology, 522.1, 165-175 They concluded that the activity of the phrenic motoneurones is organised such that it contributes to both posture and respiration during a task which repetitively challenges trunk posture. Cowan et al (2004) delayed onset of transverse abdominus in long-standing groin pain. Med Sc Sp Ex. They found that the onset of transverse abdominus was delayed in individuals with long standing groin pain. Abt JP et al (2007) Relationship between cycling mechanics and core stability. J strength and Conditioning Research, 21(4), 1300-1304 Core fatigue resulted in altered cylcing mechanics (frontal and saggital plane knee motion and frontal plane ankle motion) which may increase the risk of injury as the knee joint is exposed to greater stress. von Banchet GS et al (2009). Gisela Segond von Banchet, Michael K. Boettger, Nadja Fischer, Mieczyslaw Gajda, Rolf Bräuer, Hans-Georg Schaible (2009) Experimental arthritis causes tumor necrosis factor-alpha-dependent infiltration of macrophages into rat dorsal root ganglia which correlates with pain-related behavior. Pain, 145, 151-159. After peripheral nerve damage macrophages infiltrate the dorsal root ganglia (DRG) in which cell bodies of lesioned neurons are located. However, infiltration of macrophages into the DRGs was also reported in complete Freund's adjuvant (CFA)-induced inflammation raising the question whether CFA inflammation induces nerve cell damage or whether peripheral inflammation may also trigger macrophage infiltration into DRGs. Related questions are, first, which signals trigger macrophage infiltration into DRGs and, second, is macrophage infiltration correlated with pain-related behavior. Using the rat model of unilateral antigen-induced arthritis (AIA) in the knee we found a massive infiltration of ED1+ macrophages into the ipsi- and contralateral lumbar DRGs but not into thoracic DRGs. At no time point of AIA DRG neurons showed expression of activating transcription factor-3 (ATF3) indicating that macrophage infiltration is not explainable by nerve cell lesions in this model. During AIA, lumbar but not thoracic DRGs exhibited a bilateral de novo expression of vascular cell adhesion molecule-1 (VCAM-1) which is known to be involved in macrophage infiltration. Tumor necrosis factor-alpha (TNF-alpha) neutralization with etanercept or infliximab treatment after induction of AIA significantly reduced both macrophage infiltration and VCAM-1 expression. It also decreased mechanical hyperalgesia at the inflamed joint although the joint inflammation itself was barely attenuated, and it reduced mechanical hyperalgesia at the non-inflamed contralateral knee joint. Thus, bilateral segment-specific infiltration of macrophages into DRGs is part of an unilateral inflammatory process in peripheral tissue and it may be involved in the generation of hyperalgesia in particular on the non-inflamed side. |
|
Transverse Abdominis and Serratus Anterior - Low Back Pain and Shoulder Dysfunction Clinical Instability of the Lumbar Spine Psychosocial and Cognitive Factors Updated 13 October 2020 |
|