Clinical Reasoning for a knee - pelvic - back condition in a runner with an overactive Tranversus Abdominis and an inability to breath
by Martin Krause (2007)
Interestingly, the reduced femoral pulses reflected reduced lateral diaphragm activity and hence reduced rythmical 'pulsing' (elongation-contraction) of the iliopsoas muscles, due to excessive transverse abdominal activity in a malaligned pelvis.
This was a classic case of a 'traditional floppy' with stiff bits. Underlying those stiff bits (muscle spasms) were functional instability.
Additional intervention included rythmical oscillation exercises in standing and in the water, as well as some orthotic prescription.
Please have a look at the cycling section and pins & needles/numbness in feet for a description of some of the exercises : http://www.back-in-business-physiotherapy.com/cycling-feet-numbness
The perenial issue with people who are inherently 'floppy' is that they have the conundrum of too many choices. Unlike, the person who is inherently a 'stiffer' and gain their feedback through structures being stretched, the 'floppy' gains feedback through success or failure of functional activity. Unfortunately, in many cases this feedback may end up as an injury such as a tendonosis and/or recurrent subluxations of joints. Thus, motor learning strategies using visual, verbal, vestibular and tactile feedback are obligatory in treating a person who has apparent dyskineasia and whose past history suggests hypermobility.
See: Motor learning section on Orienteering for an explanation which considers global stability in uneven terrain using external 'feedforward' mechanisms
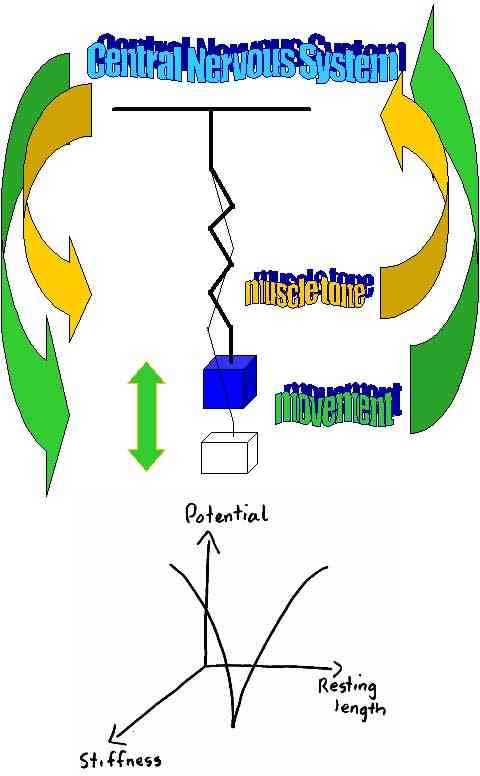
See: "Why don't our shoulders subluxate" for an explanation of the above diagram
Figure 1: A model of everything : the neuromatrix is used as a model (cognitive process oriented structure) to describe the various input which the therapist can offer to 'enable' the client to engage in their path to recovery. Hereby, an evidence based approach using 'the values and beliefs' of the client is integrated with the scientific evidence base from physiotherapy, the pain sciences and psychology. Importantly, the therapist gains confidence through their success at predictive reasoning, whilst the client gains emotional confidence in their ability to undertake goal-oriented activities without the fear of exacerbation or under-performance.
Heuristics versus Constructivism

Figure 2: A useful instructional model used to describe a 'top-down' clinical approach with a scientific clinical evidence based approach of biomechanics and neurophysiology.
Figure 3: Increasing the validity and reliability of the clinical reasoning by correlating all aspects of the subjective and physical examination into a meaningful clinical picture (pattern recognition) - adapted from Maitland (1986, 1991).
Treatment as a product of a systematic assessment
Although an at 'out of fashion' terminology, the aggravating/easing factors are a disability measure which can be used to assess the neurophysiological and biomechanical state of the pathology. By analyzing the movement and loading characteristics of the aggravating and easing factors the therapist should gain a measurable outcome tool for assessing the efficacy of treatment. Additionally, the information can be used to correlate it with impairment measures of the physical examination. Improving the internal reliability by correlating information across the entire examination process enhances the validity of your treatment and re-examination process. Ideally, the therapist should have at least 3 aggravating/easing factors to assess outcome. Otherwise, a more in depth analysis of the aggravating/easing factors should be undertaken using inductive reasoning. For example, if the client only complains of shoulder pain when lifting a load above their head, then clarify this statement by asking whether it is the movement which is painful, the duration of lifting, the manner of lifting or the size of the load which is being lifted that is significant. Night pain, the frequency of waking and the ability to return to sleep are also useful measurement tools. Psychometric disability measures can also be used if they don't result in resentment or irritation from your client.
Further aspects of the subjective examination can be used to assess the past history as it relates to the current problem. Is it the same problem re-aggravated or is it a new problem which is influenced by the old injury? Assess the biomechanical aspects of the original mechanisms of injury as well as those of re-exacerbation, as well as the frequency of exacerbation and make a judgement as to whether the problem is getting worse, better or staying the same. If it is getting worse, then why? Are there components of misuse (reduced co-ordination/stability), disuse (atrophy and reduced capacity of loading), abuse (trauma), or overuse (repetitive loading and microtrauma) which are contributing to the 'cause of the cause' of the problem. A long history of problems may identify fear-avoidance behaviour and generalised 'disuse' and/or of more specific 'disuse' of the multifidus and transverse abdominis muscles. Combine this with 'overuse' of the erector spinae muscles leading to excessive compression of the intervertebral disc and consequent neural irritation of the dorsal root ganglia resulting in ectopic impulse generation and increased muscle tone in the deep hip rotators, hip flexors, hamstring and calf muscles which creates 'misuse' of the lower limbs ('the tail that wags the dog phenomena') generating shearing and rotating forces across the pelvis.
Old injuries may not only reduce the biomechanical integrity of the tissue but it may also increase the neurophysiological sensitivity of the neurones whose nerve fibres innervate the territory of previous injury. Ascertaining the recuperation from previous injury will provide an insight into the clients 'active' and/or 'passive' coping strategies. People who have had frequent passive treatment inputs and have recovered may find it difficult to embrace a more active treatment approach. Those who haven't recovered may be in a state of 'learned helplessness' who will similarly require convincing to embark on a more active form of recuperation. Importantly, the active treatment approach must embrace the impairment and disability measures of the subjective and physical examinations, thereby allowing the client to measure success leading to the ultimate goal of full self management and/or complete recovery. Therefore, this process requires an element of education whereby the therapist's 'hands-on' treatment becomes 'exercise enabling' and/or 'performance enhancing' for the client.

























































































































