by Martin Krause
Fibromyalgia (FM), or polymyalgia, is a complex chronic pain condition. It is manifested by both peripheral and central changes in neuropeptide and immune markers. People with FM exhibit a generalised stiffness and soreness across multiple regions of the body, frequently associated with fatigue and reduced capacity to sustain postures or exercise.
This clinical manifestation can have multiple causes, some of which are clearly defined musculoskeletal dysfunction such as spinal dysfunction from degenerative joint disease. Additionally, some people present with clear auto-immune compromise such as thyroid issues, Irritable Bowel Syndrome (IBS) or blood born immune factors. However, frequently, the inflammatory aspect is sub-clinical in nature, which makes diagnosis a process of exclusion as blood results frequently come back inconclusive. Without a clear diagnosis, a musculoskeletal physiotherapist will need to take a multifactorial treatment approach, which requires a combination of musculoskeletal techniques, such as joint mobilisations, dry needling, massage, muscle energy techniques and exercise regimes, including consideration of metabolic, central nervous system and immune compromise.
Specifically, the gut - muscle immune axis plausibly has a major impact on this musculoskeletal - immune disorder. The gut biome contains species associated with energy extraction as well as species associated directly with the immune system. Both muscle and gut contain heat shock proteins and neuropeptides which play an important role in both the innate and learned immune system. Muscle mass will determine the amount and quality of protein available for the immune system. Sarcopenia, the gradual loss of muscle (apoptosis), in sedentary individuals, commences in the 4tn decade of life. Once that muscle is lost, unlike atrophy, it is lost forever, Similarly, lack of physical activity results in a less defined and hence less robust gut, leading to dysbiosis. Lack of energy and immune compromise can be the result of a sedentary lifestyle, which later in life can presumably transform or lay the foundations for vulnerability to FM. Physiotherapists, when treating FM need to consider muscle and gut as immune organs, when prescribing treatments, especially associated with exercise, otherwise a state of 'over-training' may quickly arise, leading to a further downward spiral in clinical signs and symptoms.
The brain makes the choices of what we eat, where we move to and what exercise we do. It also decides on 'stressors'. What is a 'danger signal' such as Matzinger's Danger hypothesis and what represents a 'safety signal' or beneficial stimulus. Such Allostatic Mechanisms require consideration in terms of the persons activities of daily living (ADL) and their health status.
The Hypothalamic-Pituitary-Adrenal axis is also highly likely playing a role FM not only in the post-menopausal person, but also in the over-trained and under-nourished elite athlete. In the latter, the status of the menstrual cycle should be questioned, as young female athletes have been known to suffer from irregular menstrual cycles including late onset menarche, dysmenorrhea and amenorrhea. Historically, this was also known as Adrenal fatigue.
Medical intervention, frequently involves the use of high doses (50-70mg) of steroids such as prednisone, in the acute reactive stage of the condition, which is reduced overtime to <5mg. However, long term steroid use may result in side effects such as Cushings Syndrome, which may lead to osteoporosis and type II diabetes, amongst other things. Since hormonal changes appear to be a pre-cursor to FM, any negative influences, to the already compromised, hypothalamic-pituitary-adrenal axis, should be avoided. Ideally, a multidisciplinary approach is taken, whereby the use of pharmacological intervention and it's potential side effects, can be ameliorated or minimised, through physiotherapeutic, exercise physiology and dietary considerations.
The gut - the use of exercise as a treatment consideration
People suffering from FM often find unguided and unstructured exercise too painful to undertake. Yet, exercise is known to have anti-inflammatory effects (Ortega et al 2009 Exerc Immunol Rev.15:42-65) as well as amelioration of metabolic-immune compromise. Hence, a 'happy medium' needs to be found, as exercise alone can have profound effects on the gut, which has a direct influence on the immune system
The Paper of the Year for Exercise and Sports Science (2020) was recognised for several findings, on exercise and the gut, including
- exercise alters the microbiome of the gut independently of diet
- exercise exerts strain level selection for microbes within the host more robustly than genotype
- reduced exercise tolerance in situations of reduced microbiome (eg anti-biotic use and gene knock out mice)
- mechanism is likely via butyrate-producing microbes
- gut-immune interactions via gut-associated-lymphoid tissue
- bile acid circulation
- metabolic flux
- Specifically, Fecalibacterium prausnitzii, has been shown, not only to be enhanced with exercise training, it is thought to improve type II diabetes outcomes, as well as improve symptoms of depression and anxiety. (Mailing et al 2019, Ex Sp Sc Rev, 47, 75-85).
Two symbiotic relationships exists between muscles and the gut. The most obvious one, is the relationship between energy species of the gut and the need of energy for muscles to perform work and regulate thermogenesis. However, the frequently under appreciated relationship, is that both the gut and muscle are major organs of the immune system. Both, muscles and the gut are influenced by aging. Since, the onset of FM, tends to be in the 5th and 6th decades of life, factors such as sarcopenia, the gradual loss of muscle mass after the 4 decade of life, in sedentary individuals, along with alterations in the gut biome, should be considered clinically.
The amount of human DNA is totally under-whelming compared to that of the intestinal mircobiome. The intestine is composed of a complex ecosystem of more than trillions of bacteria, viruses, fungi, Protozoa and Archea that live in a symbiosis with the host in the gut lumen. The healthy microbiome include a limited number of highly represented taxa, such as Bacteroides and Prevotella and a large number (>2000 to date) of minor players with low representation but high metabolic activity. These latter 'players' with high metabolic activity are likely to be the ones which interact with the musculoskeletal system. In older age, species richness and diversity of the microbiome decline, inter-individual variability increases, and resilience to perturbations are reduced. Apart from aging, the presence of acute and chronic diseases affects the microbiome. In the aging and/or unhealthy microbiome a 'dysbiosis' can occur, where a disruption of the gut balance 'symbiosis' results in intestinal permeability, allowing bacteria, or bacterial toxins and metabolites to enter the host circulation thereby promoting sub-clinical inflammation. Clinically, sub-clinical inflammation has been referred to as 'inflammaging' and 'immunosenescence'. Both the innate and adaptive immune system are affected by aging.
All components of the innate immune system exhibit profound changes during aging. Monocytes are classified into three subtypes: classical, non-classical, and intermediate. During aging the number of nonclassical CD14+CD16+ monocytes increases, indicating a shift to senescence, proinflammatory phenotype with short telomeres. Similarly, a shift in macrophages from immunoregulatory M2 macrophages to proinflammatory M1 macrophages. Furthermore, Natural Killer (NK) cells are innate lymphoid cells, where 2 subtypes are present. CD56bright cells are immature cells providing an immune regulatory function, and CD56dimCD16+NK cells which produce high levels of IFN-gamma, associated with a potential dysregulated cytokine production, as CD56bright cells decrease with aging. Moreover, exercise appears to have the opposite effect to aging, where a reduction the number of nonclassical CD14+/CD16+ monocytes, was found, in a 12 week combined strength and endurance training program.
The adaptive immune system changes with aging. Although the total number of T-cells remains constant throughout life, the two main cellular subtypes CD8+ cells increase, whereas CD4+ decrease. This phenomenon is part of the immune risk profile (IRP) and indicates immunosuppression in certain diseases. Reduction of naive CD4+ cells is driven by thymic involution from chronic antigenic stimulation and inflammation. Inflammaging chronically increases IL-6 and TNF-alpha. Improved T cell function has been reported in elderly runners who trained for an average of 17 years, and thus improvements in the adaptive immune response. In 102 male participants between 18 and 61 years of age, with above-average VO2 had fewer senescent CD28-CD57+, CD4+, and CD8+ cells and increased number of naive CD8+ T cells. Acute bouts of exercise induces cell death in apoptosis-resistant senescent T-cells. Moreover, regular endurance training in the elderly, improves CD4+/CD8+ ratio. Although exercise seems to improve the immune system, endurance exercise seems better than strength training alone.
Exercise also influences inflammation induced from visceral adipose tissue (fat). Toll-like receptors (TLRs), mainly in the innate immune system, are upregulated with physical inactivity, systemic inflammation and the development of age-related diseases. They are particularly reactive to heat shock proteins (HSP). HSP's are found in muscle and released with exercise. Conversely, a reduced expression of TLR2 and TLR4 has been found in both acute and regular exercise. Importantly, skeletal muscle itself acts as an endocrine organ, whereby muscle contractions and energy metabolism induce the production of various cytokines-termed myokines-or peptides with anti-inflammatory potential. As highlighted earlier IL-6 is one of the most effective myokine. IL-6 increases during and after exercise, proportional to intensity and duration, stimulating immune-regulatory mediators such as IL-10 and the IL-1 receptor antagonists and downregulation of TNF-alpha by monocytes and macrophages. Results from middle-aged master athletes demonstrated that IL-1ra, IL-1beta, IL-4 and IL-8 levels were elevated compared to inactive, younger-middle-aged controls. Exercise-induced IL-6 has been shown to inhibit endotoxic-induced TNF-alpha. Besides IL-6, myokines such as meteorin-like has been shown to induce brown fat metabolism, increase IL-4 levels and promote polarization of M2 macrophages. IL-7 and IL-15 are myokines that might stimulate lymphocyte proliferation and it has been suggested that IL-7 exerts protective effects on the thymus.. IL-15 seems to have further effects on immune homeostasis which induces a better survival rate of naive T-cells. At a metabolic level, IL-15 reduces the accumulation of visceral and white adipose tissue by reducing the accumulation of fat.
Exercise is generally considered a positive modulator of the gut biome. Regardless of age, exercise has a positive effect on taxa involved in energy, carbohydrate and protein metabolism and short chain fatty acid (SCFA) production. Maintenance of exercise is needed to induce long-lasting modifications of intestinal microbial ecosystem. Such changes have been shown to improve the inflammatory mediators of the gut. Importantly, dosage of exercise is critical, as over-exercise can induce ischaemic events in the gut mucosa, associated with acute gastrointestinal symptoms including abdominal pain, nausea, and diarrhoea. Supplementations, of probiotics and prebiotics can attenuate some of these unfavourable changes of the gut. Care is also needed when taking mineral or energy supplements, as these may also have negative effects taken at the wrong dose.
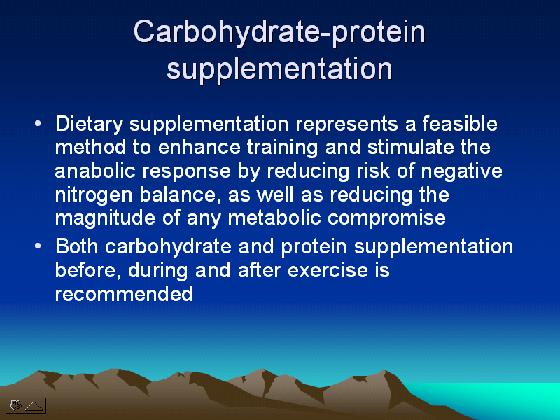
Dietary supplementation would plausibly have an impact on enhancing the effect of training, in addition to reducing the impacts of potential 'over-training'. Probiotics have been shown to modify the gut microflora population, increase natural killer (NK) cell cytotoxicity, increase secretary immunoglobulin A (IgA) levels, and enhance resistance to infections, potentially through the kynurenine/tryptophan ratio, activated T-suppressor (CD8+CD25+) and natural killer cells (CD56+CD16+) in high doses, whilst low doses increased activated T-helper lymphocytes (CD4+CD25+), B-lymphocytes (CD19+) and antigen-presenting cells (HLA-DR+). Common examples of Pro-biotics include some diary products and pickled foods such as Sauerkraut and Kimchi.
Glucose and fructose hydrogels have been demonstrated to enhance running performance, exogenous CHO oxidation and gastrointestinal tolerance (Rowe JT et al 2022 Med Sc Sp Ex, 54, 1, 129-140). High fat diets also have a tendency to gastrointestinal motility issues which may be detrimental to exercise performance.
Sarcopenia, metabolic compromise and the gut biome
There is a gut-muscle axis hypothesis in age-related sarcopenia. A dysbiotic intestinal microbiota can effectively result in reduced bio-availability of dietary proteins, in particular tryptophan, which is a powerful mediator of inflammation, as well as a promotor of muscle protein synthesis. Additionally, the gut bacteria are also involved in the synthesis of many vitamins, including folate, vitamin B12 and riboflavin, which exert pro-anabolic effects on muscles.
Tryptophan is a pre-curser of serotonin and plays a pivotal role in immune system regulation. Enhanced breakdown of the tryptophan kynurenine pathway occurs in aging and in conditions with an increased pro-inflammatory response. Tryptophan and in particular serotonin have been known to be associated with mood and cognition. The kynurenine pathway not only plays a role in the innate immune system via IDO (an enzyme which degrades tryptophane) and it's influence on IFN-gamma, but also in the adaptive T-cells immune response, through selective apoptosis of Th1, and not Th2, cells. Accumulating evidence implicates gut microbiota in the regulation of kynurenine pathway metabolism, and thus the gut-brain axis. Chronic exercise interventions may lead to reductions in IDO activity as a result of anti-inflammation.
Assuming that chronic inflammation induces sarcopenia and vice versa, meaning that good muscle mass reduces chronic inflammation, a vicious cycle needs to be broken by any means possible, through a combination of dose specific exercise and diet. As already stated anti-oxidants and sufficient carbohydrates and protein are important in our diets. Additionally, n-3 polyunsaturated fatty acids (PUFAs), has been shown to have anti-inflammatory properties through their effect on leukocyte action, eicosanoid production, and T-cell proliferation. PUFAs in combination with strength and endurance training have been shown to have favourable muscle building effects, where 6 months of Progressive Resistance Training (PRE) (2 x week, 3 sets per x's. 50-85% 1RM) combined with n-3-PUFA-rich diet, improved gene expression, whereby pro-inflammatory IL-1beta was down-regulated and regulator of cellular growth mechanistic Target of Rapamycin (mTOR) was up-regulated in skeletal muscle in older women.
Exercise training has been shown to reduce intestinal inflammation and modulate gut microbiota profiles in insulin-resistant people (Motiani et al 2020, Med Sc Sp Ex, 52, 1, 94-104), using both moderate-intensity continuous training (MICT) and sprint interval training (SIT). High fat diets reduces the Bifidobacterium, Eubactterium rectale-Blautina coccoides, and Bacteroides genus which leads to an increase in the Gram-negative : Gram positive ratio, meaning a subsequent increase in LBP {Metabolic endotoxemia (LPS binding protein [LBP])} was found by Cani et al (2008 Diabetes, 57, 6, 1470-1481). Moliani et al (2020), on the other hand, found the opposite with both forms of exercise training. There was a reduction in Firmicutes/Bactroidetes ratio, mainly due to an increase in the relative abundance of Bacteroidetes and a decrease in abundance of Blautia spp. and Clostridium spp at genus level. This may induce regulatory T-cells to produce IL-10 (anit-inflammatory cytokine) inside the gut (Mazmaniian et al 2008 Nature, 453, 7195, 620-625). Furthermore, it was found that Bacteroidetes at the species level correlated negatively with plasma inflammation (LBP, TNF alpha, and CRP levels) (Moliani et al (2020). Exercise training also reduced the relative abundance of Clostridium and tended to reduce the Blautia genus. The former thought to play a role in whole body inflammatory response and the latter found in abundance in pre-diabetic people. Moliani et al (2020) also found a reduction in TNF alpha after 2 weeks of training, which also plays a critical role in inflammation. The Firmicutes/Bacteroidetes ratio is elevated in obese people, whereas it is reduced in this study as well as in some investigations examining dietary intervention.(Ley ey al 2006 Nature, 444, 7122, 1022-3)..It is thought this ratio is important in that Firmicutes may contribute to obesity because they can harvest more energy from food (Turnbaugh et al 2008, Cell Host Microbe, 3, 4 213-223). Increases in faecal Bacteroidetes were also found, which is significant as it plays an essential role in the metabolic conversions of complex sugar polymers and degradation of proteins (Rajilic-Stojanovic & Voss 2014, FEMS Micorbiol Rev, 38, 5, 996-1047). Although, these are very positive findings for exercise intervention, chaos theory would suggest that the SIT group should have shown more changes than the MICT group.
References
Weyh C et al (2020), Nutrients, 12, 622: doi:10.3390/nu12030622
Ticinesi A et al (2019) EIR 25, 84-95
Ticinesi A et al (2019) Nutrients, 11, 1633; doi:10.3390/nu11071633
Codella et al (2017), Digestive and Liver Disease, doi:10.1016/j.dld.2017.11.016
Dietert R & Dietert J (2012), Entropy, 14, 2036-2065: doi:10.3390/e14112036
Treatment - the use of supplements
Experienced physiotherapy practitioners are realising the use of nutritional supplementation emphasises an holistic approach to the treatment of musculoskeletal injuries which results in quicker recovery, enhanced functioning as well the prevention of further injury.
Glucosamine (1200mg) and chondroitin sulphate (800mg) combine with methylsulfonylmethane (MSM) (800mg) are considered important in improving the production and/or size of hyaluronic acids as well as regulating the expression of matrix-degrading enzymes and their inhibitors. Furthermore, the concentration of sulphur in arthritic cartilage has been shown to drop to 1/3, thereby suggesting a role for MSM supplementation. High quality fish oils with an EPA and DHA concentrations of at least 1000mg is thought to have an inhibitory effect on arachidonic acid metabolism (Petra Hunt 2012, FX Medicine, 66, 10-11). Furthermore, fish oils anti-oxidation effect and it's balancing effect on hyper-lipidemia suggests that it may have a role to play in tendon degeneration where immune-metabolic compromise has been found to be an important aspect of tendon degeneration and necrosis (see shoulder section elsewhere on this site). CoQ10 is also thought to help in the reduction of cholesterol and the enhancement of mitochondrial oxidative activity which, presumably, would also be good for skeletal muscles and tendons. Fish oils have also been associated with cognitive functioning, whose compromise can lead to irritability, depression and reduced immune function.
Compromised intestinal barrier function in people with food intolerances has been associated with inflammation at extraintestinal sites, including the joints. Evidence supports the relationship between the gastrointestinal microbiota, the mucosal and systemic immune responses and the development of arthritis. In fact glucosamine has been shown by A/Prof Luis Vitetta (Uni Qld) to have more favourable effects in patients with larger amounts of favourable enteric bacteria. Some new therapies include the use of pro-biotics in the treatment of joint disease. Treatment of fibromyalgia has included the use of supplements such as Vitamin D, magnesium, malic acid and acetyl-L-Carnitine (Leng 2012, FX Medicine, 66, 16-17).
Carbohydrate supplementation
Carbohydrate (CHO) appears to be an important energy source for athletes not wishing to compromise their immune system. Investigations, have shown, that short-term adherence to a low CHO high fat diet (LCHF) results in small, yet unfavourable iron, immune, and stress responses to exercise (McKay AKA et al 2022 Med Sc Sp Ex, 54, 3, 377-387), This result was CHO, not energy dependent, raising serious concerns about prolonged exposure to ketogenic diets.
Clinical Reasoning in Musculoskeletal Physiotherapy on Nutritional Supplementation in Sport and Disease
Exercise Regimes
Progressive Resistance Training (PRT) to gain muscle mass
Exercise - a multimodal approach to gaining endurance
Exercise programmes may need to be modified and adapted to improve compliance through reduction in micro-trauma occurring in certain forms of exercise. Since endurance exercise is recommended, then fatigue levels need to accounted for and the usual timeframe of 12-16 weeks to build up 'resistance to fatigue', may take a lot longer and require a multimodal exercise approach. For example, warm water hydrotherapy and sometimes post exercise cold water therapy is generally better tolerated than suddenly taking on running, in the novice or in someone suffering from FM. Additionally, cycling is generally considered easier on the body than running. As already stated, some resistance weight training may need to undertaken in the presence of sarcopenia.
Hydrotherapy
Hydrotherapy can be a very 'fun oriented' group activity. Since FM, has such a chronic debilitating effect on some people, the idea of exercise, which is non-threatening (Mazingers Danger Hypothesis), low loading and encourages a 'group dynamic' can be very beneficial for the central nervous system components of pain generation and modulation. Furthermore, the buoyancy and resistance elements of water, allow for greater ranges of motion, massaging effects, pressure differentials conducive to lymphatic drainage, metabolic stimulation, as well as effects of the warmth of the water on Heat Shock Proteins (HSP). The latter being the basic building blocks of life on this planet and in terms of healing, the instigators and gate keepers of repair.

Read more : Hydrotherapy for Core Stability
Matzingers Danger Hypothesis and Allostasis
Whole Body Vibration Therapy
Whole body vibration (WBV) has been shown to increase blood BDNF levels, with concomitant improvement in lower limb muscle strength, aerobic capacity, clinical symptoms and quality of life in women with FM (Ribeiro VGC et al 2022 J Healthcare Engineering). Read more on WBV here
Cycling vs Running
Interestingly, in the investigation cited above, by choosing a cycling program, any effect of muscle micro-tears and an immune response is mitigated, as would be seen with eccentric exercises, such as a running regime. Hence, this is a purely metabolic (vs mechanical) load, where the SIT is high intensity but of a much shorter duration (30secs x 4-6 bouts) vs MICT of 40 - 60 minute duration. One would surely elicit an anaerobic, lactic acid, response whilst the latter would elicit a Glut-4 muscle energy metabolising response. It's difficult to reconcile this on a purely metabolic basis and perhaps it's the neural activation of exercise which is the prime signalling pathway? WBV may be the medium in between the two forms of exercise.
Neurophysiology of pain - the central nervous system and immune response
Clearly, to understand fibromyalgia, beyond gut-muscle-immune interactions, we need to also examine the mechanisms of pain.
Hyperexcitability of the central nervous system due to activation of muscle nociceptors results in
- increased background neuronal activity
- increased responsiveness of the peripheral nerve
- appearance of new receptive fields (within minutes) in cortical areas
- spread of excitation to other spinal segments
Neurotransmitters and neuropeptides involved in myositis induced central sensitization include
- the activation of NMDA and NK-1 receptors which allows the expansion of the spinal target area (Hoheisel et al 1997)
- increased background activity in the dorsal horn due to the release of NO (nitrous oxide)
- Glutamate release magnesium which allows the influx of calcium. Na channels and AMPA/KA becomes active. NK1 cells are stimulated by substance P.
- Brain Derived Neurotrophic Factor (BDNF) activates TrkB receptors which stimulates PKA and PKC (protein kinase) release and phosphorylation (Mense & Hoheisel 2008)
Read more : Pain in the Brain
Glial cells affect central sensitization through
- the release of pro-inflammatory cytokines, IL-1, TNF-alpha, BDNF - see Neuro-immuno-cognitive section of this website
Central sensitization induced by Nerve Growth Factor (NGF) which causes
- 'sterile inflammation' since it's release does not cause acute pain but does create long-lasting increase in subthreshold background activity leading to allodynia and hyperalgesia. This may be particularly important in repetitive occupations and in musicians. (Svensson et al 2003, Mense & Hoheisel 2008)
- NGF is likely to be involved with DOMS (Graven-Nielsen & Arendt-Nielsen 2008)
- alteration in cortical excitability was found in people with FM and is associated with deficits in intracortical modulation involving both GABAergic and glutamatergic mechanisms, possibly related to certain aspects of the pathophysiology of this chronic pain syndrome (Mhalla A et al 2010 Pain, Volume 149, Issue 3, Pages 495-500)
Tissue Acidosis
- low pH activates acid-sensing ion channels (ASICs). ASIC3 plays a key role in mechanical hyperalgesia induced my muscle insult. ASIC3 is found in DRG (dorsal root ganglion) innervating muscles (Sluka et al 2003). Application of pro-inflammatory cytokines (NGF, serotonin, IL-1beta, prostaglandin E2, bradykinin) to DRG cells mimics the increased ASIC3 mRNA seen after inflammation. Sluka et al (2007) concluded that activation of ASIC3 in the primary afferents innervating muscle is critical for the development of central sensitization after muscle insult and for consequent mechanical hyperalgesia.
Cytokines act on inflammation and repair through
- the balanced release between pro and anti-inflammatory cytokines
- soluble receptors (TNFsRII, IL-1RSII)
- decoy receptors (IL-1RII) (Kopp & Alstergren 2008)
Sympathetic nervous system
- descending modulation
- genetic phenotypes predisposing to pain include a common single nucleotide polymorphism (SNP) in codon 158 of the COMT gene and has been associated with the perception of pain in humans (Zubieta et al 2003)
- inhibition of COMT (catechol-O-methyl transferase), a key enzyme which metabolizes catecholamines (adrenaline, noradrenaline) induces mechanical and thermal hyperalgesia and produces proinflammatory cytokines in rats. Blockade of Beta-adrenoreceptors diminishes clinical pain reported in a subpopulation with TMJD and FMS (Maixner 2008). This also reverse the suppression of the HPA axis (see below) by increasing the secretion of cortisol (Kizildere et al 2003)
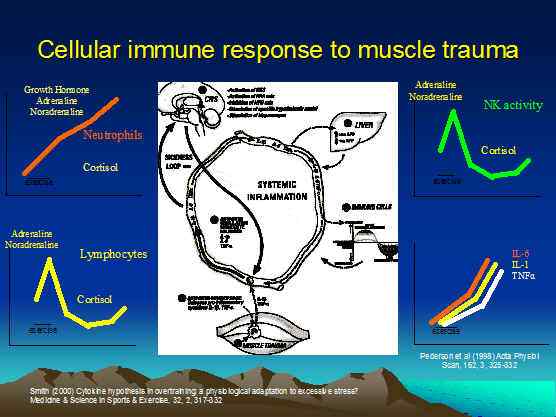
- Muscle trauma from a bout of severe acute resistance training, in a group of well trained Finnish men and women, was shown to induce a neuroendocrine and immune systems response. Specifically, Leukocyte Beta-2-Adrenergic receptor expression was elevated on monocytes and granulocytes during the exercise, and elevated on lymphocytes during the recovery phase. These responses were thought to be under the control of adrenaline (epinephrine) and noradrenaline (norepinephrine) from peripheral sympathetic nerve terminals (Fragala et al 2011, Med Sc SP Ex, 43, 8, 1422-1432)
Pain Adaptation Model
- Lund et al (1993) suggested the pain-adaptation model to explain the interrelationship among activity in nociceptor afferents, a central pattern generator, motor function and co-ordination of muscles. This pain-adaptation model predicts increased muscle activity in the agonistic phases during muscle pain, thereby decreasing movement amplitude and velocity
Cerebral Processing of Muscle Pain
- prominent activation of the cerebellum and anterior cingulate cortex (ACC) and primary somatosensory cortes (S1) during muscle pain (Svensson et al 2008)
- increased 'interoception' via the right insular subserving the limbic sensory system (traditionally associated with emotion)
- the ACC has been associated with pain unpleasantness, with attention to pain, and with the motor component to the pain response (Apkarian et al 2005). The mid cingulate and more rostral perigenual activation is associated with the cognitive and affective divisions of the ACC resp (Bush et al 2000).
Multimodal approach to treating musculoskeletal conditions
The pain (central and peripheral, neurophysiological and immune) mechansims need to be understood, by the treating practitoner, if the appropriate intervations are to be applied.
Read more on clinical reasoning here
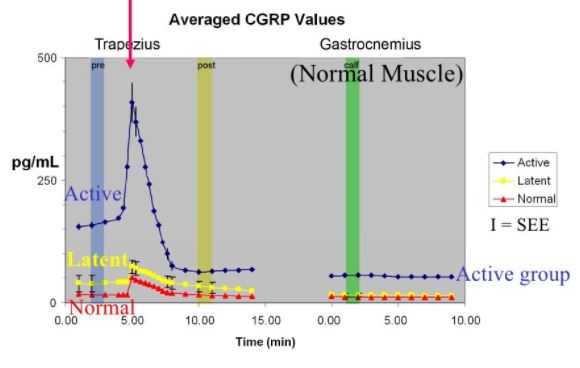
Treatment - the use of soft tissue techniques
Several soft tissue techniques are available to the physiotherapist. These include myofascial releases, trigger point therapy using massage and/or dry needling. Trigger points are an area of muscle which has been hypersensitised as a result of neuro-immune substances being released into an area. This can lead to increased muscle tension and spasms.
This hypersensitivity is not only represented by local tenderness, it can also present as referred pain into another part of the extremity.
Amazingly effective, trigger point massage can be excruciatingly painful when applied correctly and gently, but within 15-30 seconds the pain should wear off and the underlying tension should reduce dramatically. Emphasis should be on the circular technique and not a lot of force should be required. A therapist should be able to use their 'pinky' finger when applied correctly. If this technique doesn't result in reduced tension within 3 minutes, I suggest dry needling should be used, so long as the client has no phobia for needles. I generally massage the area with arnica cream beforehand, which usually means that the patient doesn't feel the needle at all.
Further techniques applied to the myofascia, might include 'releases' followed by kinesiotape. The reduction in tension should last for 48 hours purely from an immune neurophysiological cascading mechanism. However, the new threshold of 'relaxation' can allow for new 'motor programmes' to be laid down, making exercising easier.

Myofascial Trains
Kinesiotape

Manual Therapy
Manual therapy or joint mobilisations can be used to reduce pain and stiffness. This is particularly useful in people whose FM is induced by joint pathology. Another form of joint mobilisation is mechanical traction, whereby neural irritation from spinal column compromise or thoracic ring dysfunction can be addressed.
Determination of dose, using mechanical traction is very important. In my experience, normalisation of signs and symptoms can occur with as little as 6kg and usually doesn't involve a load greater than 14kg. More force, probably leads to increased spasms. Less is more
Read More : Mechanical Traction
The use of oscillatory treatment techniques in physiotherapy
A 'deterministic chaos' approach to theoretical reasoning suggests that a new oscillatory pattern can 'dampen' or 'enhance' pre-existing' oscillatory patterns. Interestingly, the Australian, Geoff Maitland approach to Musculoskeletal Physiotherapy, uses oscillatory joint mobilisations to reduce pain and muscle spasms, which in turn increases pain-free range of motion. Other oscillatory modalities used by physiotherapists include Ultrasound, Whole Body Vibration, and exercise regimes.
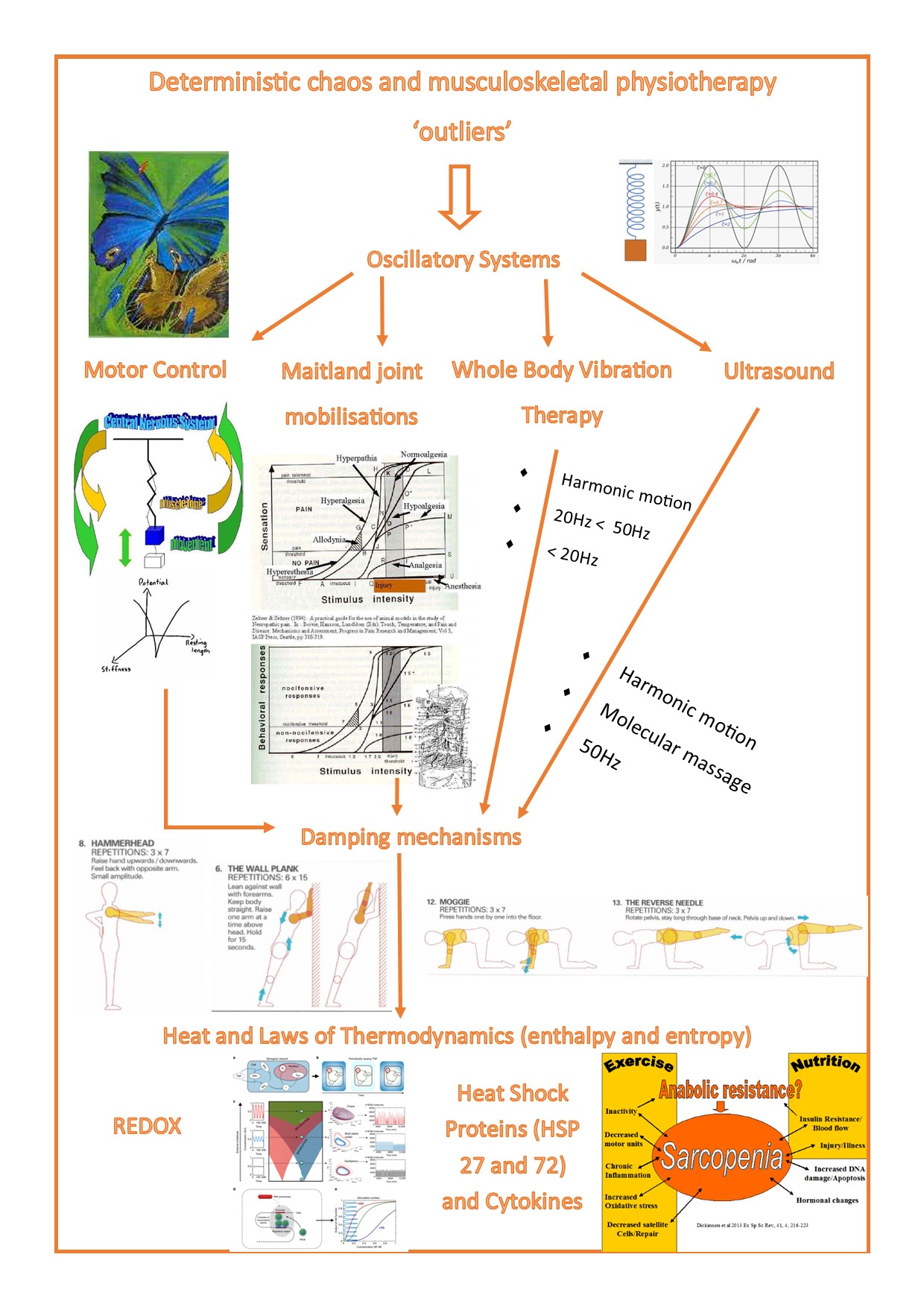
Read more on Deterministic Chaos here
Fibromyalgia - chronic fatigue flow chart in the young sporting female athlete
During my time as a physiotherapist to elite and professional athletes (Switzerland 1988-1993), I noticed that many young women had bone 'stress fractures'. A combination of factors were at play. The winter, resulted in harder ground and lack of sun reduced Vit D levels. Additionally, lack of calorific and protein intake, and excessive prolonged bouts of exercise were leading to dysmenorrhea and even amenorrhea in girls and women under 30 years of age. Clinically, apart from stress fractures, they presented with stiffness and soreness of muscles similar to features seen in FM. Liaising with doctors, coaching staff, sports psychologist, dietician and the competition events management were required to address such a complex multi-factorial issue.
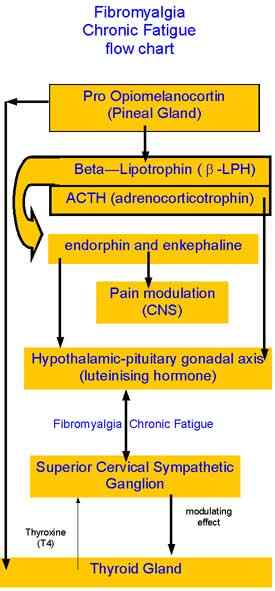
Conceptualised in Basel, Switzerland during 1991 (see references below)
Hypothalamic - pituitary axis
- Fibromyalgia, chronic fatigue and stress fractures (osteoporosis) may be the result of altered function of the gonadal-pituitary axis.
- Specifically, reduced response of the axis to stressors can result in alterations in hormonal responses during the luteal phase of the menstrual cycle.
- People particular thought to be at risk are girls that have had amenorrhea, dysmenorrhea and/or late onset of menarchy. A reduced catecholamine response has been found in female athletes with amenorrhea (Schaal K et al 2011 (Medicine & Science in Sports & Exercise. 43(1):34-43)
Predicting the failure of disc surgery by a hypofunctional HPA axis: evidence from a prospective study on patients undergoing disc surgery
Andrea Geiss, Nicolas Rohleder, Clemens Kirschbaum, Klaus Steinbach, Heinz W. Bauer and Fernand Anton
Abstract
Patients with postoperative ongoing sciatic pain have been shown to exhibit reduced cortisol levels along with enhanced IL-6 levels. The aim of the present study was to clarify the relationship between a reduced cortisol secretion and enhanced cytokine levels by performing a prospective study on patients with disc herniation. Twenty-two patients were examined before and after their disc surgery. Twelve healthy, pain-free subjects matched for age, education and gender constituted the control group. The preoperative examinations included the assessment of the diurnal pattern of cortisol secretion and the feedback sensitivity of the hypothalamus-pituitary-adrenal (HPA) axis. Patients' subjective stress levels also were assessed during the preoperative examination. The diurnal pattern of cortisol secretion was again assessed during the postoperative examination. Furthermore, blood samples were collected to measure catecholamine, adrenocorticotropic hormone (ACTH)- and interleukin-6 (IL-6) levels before and after measuring the pressure pain thresholds (PPTs). An assessment of the sensitivity of circulating monocytes to the immunosuppressive effects of glucocorticoids was further included in the postoperative examinations. Failed back syndrome (FBS) patients ( n =12) showed a reduced cortisol secretion in the morning hours and enhanced feedback sensitivity of the HPA axis. Furthermore, FBS patients displayed an increased in-vitro production of proinflammatory cytokines and a relative glucocorticoid resistance of pro-inflammatory cytokine producing monocytes as compared to non-FBS patients ( n =10) and controls. After PPT measurement FBS patients exhibited an increased norepinephrine but decreased epinephrine response, together with lower ACTH levels and a four times higher plasma IL-6 response. These findings suggest that chronically stressed patients are at a higher risk for a poor surgical outcome as their reduced cortisol secretion promotes the postoperative ongoing synthesis of proinflammatory cytokines.
Keywords: Sciatic pain; Hypothalamus-pituitary-adrenal axis; Localized glucocorticoid resistance; Proinflammatory cytokines; Chronic stress
PET imaging of hypothalamus and pain
Thyroid gland
Do high TSH values protect against chronic musculoskeletal complaints? The Nord-Troendelag Health Study (HUNT)
Knut Hagen, Trine Bjoro, John-Anker Zwart, Sven Svebak, Gunnar Bovim and Lars Jacob Stovner
Abstract
The aim of this large cross-sectional population-based study was to examine a possible positive or negative association between thyroid dysfunction and chronic musculoskeletal complaints (MSC). Between 1995 and 97, all 94,197 adults in Nord-Trondelag County in Norway were invited to participate in a health survey. A total of 64,787 (69%) responded to questions related to MSC, whereof thyroid-stimulating hormone (TSH) was measured in 34,960 individuals. These included a 5% random sample of women and men 20 - 40 years of age ( n =2165), nearly all women above 40 ( n =19,308), a random sample which included 50% of men older than 40 years ( n =9983), and 3504 (97%) with self-reported thyroid dysfunction. Among the 64,787 participants, 30,158 (47%) who reported MSC continuously for at least 3 months during the past year where defined as having chronic MSC. Associations between thyroid dysfunction and chronic MSC were assessed in multivariate analyses, estimating prevalence odds ratios (ORs) with 95% confidence intervals (CIs). High TSH values were associated with lower prevalence of chronic MSC at ten anatomical sites among women with no history of thyroid dysfunction. Among these, chronic MSC was less likely (OR=0.6, 95% CI 0.4?0.8) if TSH =10 mU/L than in women with normal TSH (0.2 - 4 mU/L). Chronic MSC was less likely among women with high TSH values. The mechanism is unclear and, theoretically, may reflect a fundamental gender-specific relationship between TSH and pain perception in the central nervous system. Pain (2005), 113, 416-421
Conclusion
FM is a complex and challenging immune - musculoskeletal clinical presentation, which requires a multi-modal and multi-disciplinary approach to treatment. Musculoskeletal Physiotherapy, using a 'clinical reasoning' paradigm, should take a 'bottom up' and 'top down' approach. Both the peripheral manifestation of the ailment as well as it's cognitive compromise are addressed using a multifactorial approach, ranging from joint mobilisations and soft tissue techniques, to exercise regimes, based on biomechanical, neurophysiological and cognitive behavioural paradigms. Moreover, the over-riding immune compromise suggests that the gut biome must be considered within the context of the relationship with muscle being seen as an organ of the immune system. Apart from Musculoskeletal Physiotherapy, treating the gut-brain-muscle axis may also involve other professionals such a nutritionists, doctors, exercise physiologists and psychologists with an interest in complex musculoskeletal dysfunction.
References
Apkarian et al (2005) Human brain mechanisms of pain perception and regulation in health and disease. Eur J Pain, 9, 463 to 484
Bush et al (2000) Cognitive and emotional influences in the anterior cingulate cortex. Trends Cogn Sci, 4, 215 to 222
Ernberg (2008) Serotonergic receptor involvement in muscle pain and hyperalgesia. In Fundamentals of Musculoskeletal Pain, ch10, IASP Press, Seattle
Graven-Nielsen & Arendt-Nielsen (2008) Human models and clinical manifestations of musculoskeletal pain and pain-motor interactions. In Fundamentals of Musculoskeletal Pain, ch11, IASP Press, Seattle
Hoheisel et al (1997) Myositis-induced functional reorganisation of the rat dorsal horn: affects of spinal superperfusion of antagonists to neurokinin and glutamate receptors. Pain, 1997, 69, 219 to 230.
Kizildere et al (2003) During a Corticotropin-releasing hormone test in healthy subjects, administration of a beta-adrenergic antagonist induced secretion of cortisol and dehydroepiandrosterone sulfate and inhibited secretion of ACTH, Eur J Endocrinology, 148, 45 to 53
Kopp & Alstergren (2008) Peripheral aspects of cytokines in musculoskeletal pain. In Fundamentals of Musculoskeletal Pain, ch9, IASP Press, Seattle
Lund et al (1993) The relationship between pain and muscle activity in fibromyalgia and similar conditions. In Vaeroy & Merskey. Progress in fibromyalgia and myofascial pain. Amsterdam, Elsevier, 311 to 327.
Maixner (2008) Biopsychological and genetic risk factors for TMJ disorders and related conditions. In Fundamentals of Musculoskeletal Pain, ch17, IASP Press, Seattle
Mense & Hoheisel (2008) Mechanisms of cnetral nerous hyperexcitability due to activation of muscle nociceptors. In Fundamentals of Musculoskeletal Pain, ch5, IASP Press, Seattle
Sluka et al (2003) Chronic hyperalgesia induced by repeated acid injections in muscle is abolished by the loss of ASIC3, but not ASIC1. Pain, 106, 229 to 239.
Sluka et al (2007) ASIC3 in muscle mediates mechanical, but not heat, hyperalgesia associated with muscle inflammation. Pain, 129, 102 to 112.
Svensson et al (2003) Injection of NGF into human masseter muscle evokes long-lasting mechanical allodynia and hyperalgesia. Pain, 104, 241 to 247.
Svensson & Abrahamsen (2008) Central representation of muscle pain and hyperalgesia. In Fundamentals of Musculoskeletal Pain, ch12, IASP Press, Seattle
Zubieta et al (2003) COMT val158met genotype affects mu-opioid neurotransmitter responses to a pain stressor. Science, 299, 1240 to 1243.
Last update : 16 May 2022