Is your child suffering Ehlers Danlos Syndrome? Hypermobile joints, frequent bruising, recurrent sprains and pains? Although a difficult manifestation to treat, physiotherapy can help.
Joint Hypermobility Syndrome (JHS)
by Martin Krause
B.Appl.Sci. (Physiotherapy); M.Appl.Sci (Manipulative Physiotherapy), Post Grad Dip Hlth Sc (Exercise and Sports), Post Grad Cert Hlth Sc (Education)

When joint hypermobility coexists with arthralgias in >4 joints or other signs of connective tissue disorder (CTD), it is termed Joint Hypermobility Syndrome (JHS). This includes conditions such as Marfan's Syndrome and Ehlers-Danlos Syndrome and Osteogenesis imperfecta. These people are thought to have a higher proportion of type III to type I collagen, where type I collagen exhibits highly organised fibres resulting in high tensile strength, whereas type III collagen fibres are much more extensible, disorganised and occurring primarily in organs such as the gut, skin and blood vessels. The predominant presenting complaint is widespread pain lasting from a day to decades. Additional symptoms associated with joints, such as stiffness, 'feeling like a 90 year old', clicking, clunking, popping, subluxations, dislocations, instability, feeling that the joints are vulnerable, as well as symptoms affecting other tissue such as paraesthesia, tiredness, faintness, feeling unwell and suffering flu-like symptoms. Autonomic nervous system dysfunction in the form of 'dysautonomia' frequently occur. Broad paper like scars appear in the skin where wounds have healed. Other extra-articular manifestations include ocular ptosis, varicose veins, Raynauds phenomenon, neuropathies, tarsal and carpal tunnel syndrome, alterations in neuromuscular reflex action, development motor co-ordination delay (DCD), fibromyalgia, low bone density, anxiety and panic states and depression. Age, sex and gender play a role in presentation as it appears more common in African and Asian females with a prevalence rate of between 5% and 25% . Despite this relatively high prevalence, JHS continues to be under-recognised, poorly understood and inadequately managed (Simmonds & Kerr, Manual Therapy, 2007, 12, 298-309). In my clinical experience, these people tend to move fast, rely on inertia for stability, have long muscles creating large degrees of freedom and potential kinetic energy, resembling ballistic 'floppies', and are either highly coordinated or clumsy. Stabilisation strategies consist of fast movements using large muscle groups. They tend to activities such as swimming, yoga, gymnastics, sprinting, strikers at soccer.

Treatment
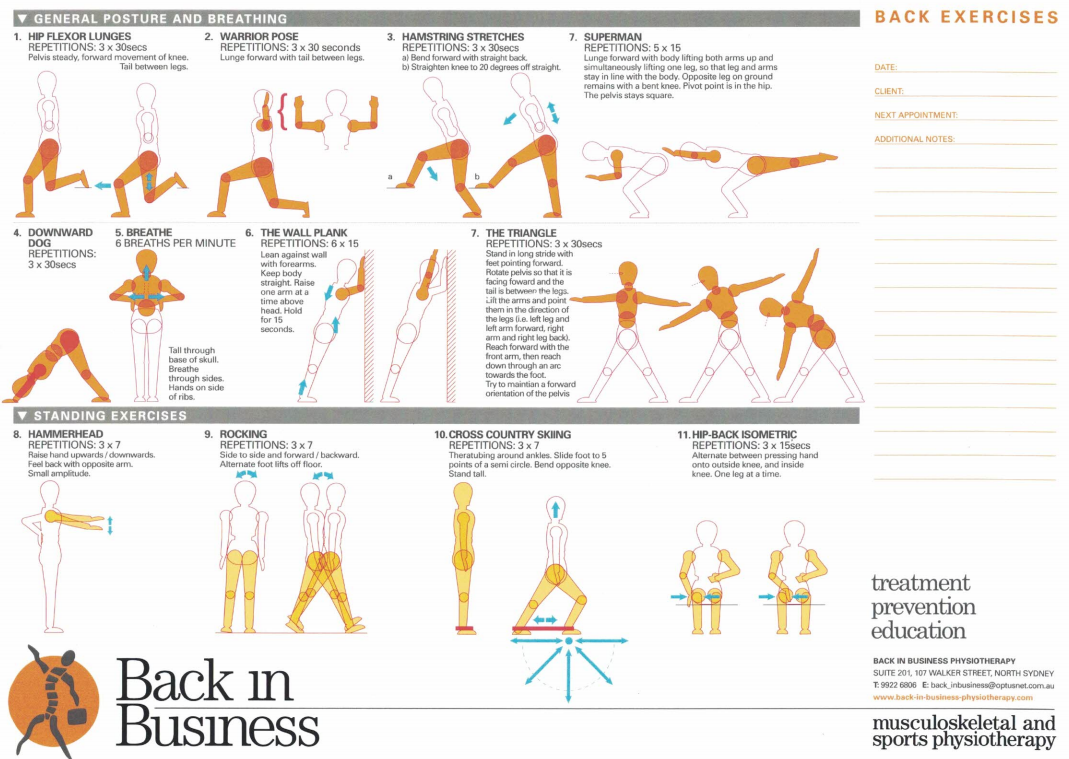
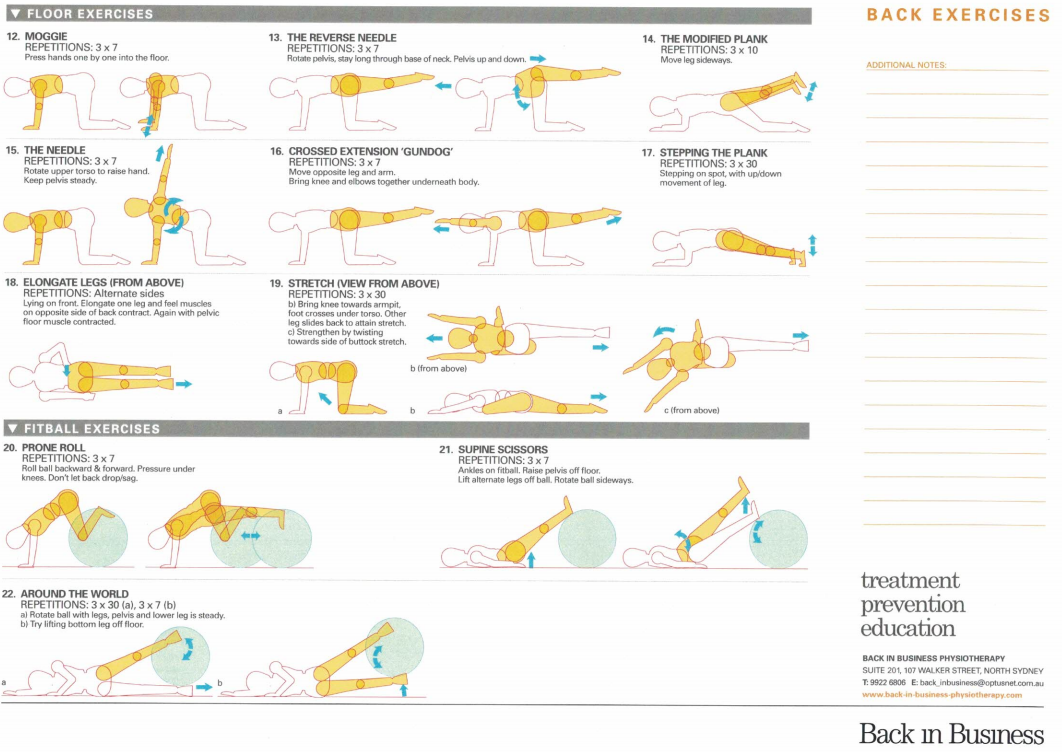
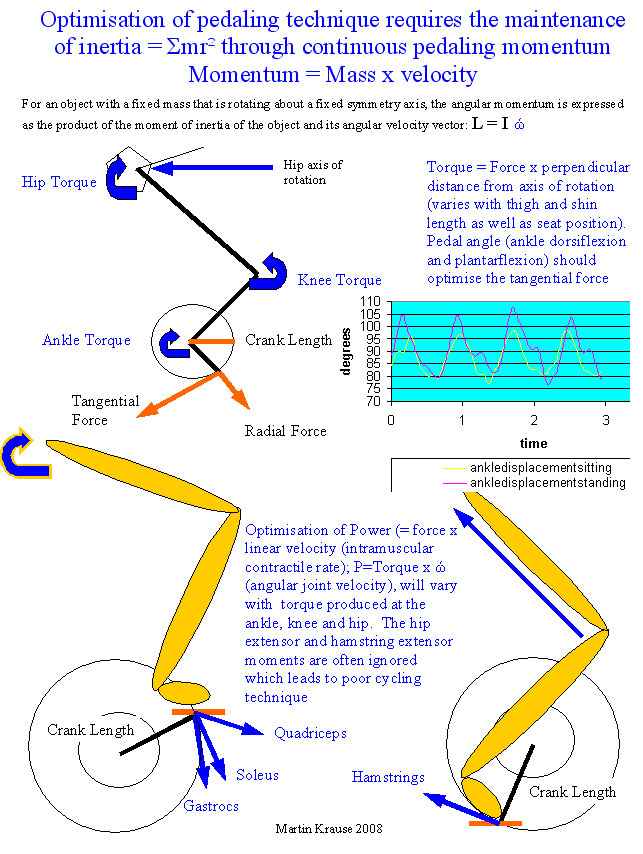
Treatment has consisted of soft tissue techniques similar to those used in fibromyalgia, including but not limited to, dry needling, myofascial release and trigger point massage, kinesiotape, strapping for stability in sporting endeavours, pressure garment use such as SKINS, BSc, 2XU, venous stockings. Effectiveness of massage has been shown to be useful in people suffering from chronic fatigue syndrome (Njjs et al 2006, Man Ther, 11, 187-91), a condition displaying several clinical similarities to people suffering from EDS-HT. Specific exercise regimes more attuned to co-ordination and stability (proprioception) than to excessive non-stabilising stretching. A multi-modal approach including muscle energy techniques, dry needling, mobilisations with movement (Mulligans), thoracic ring relocations (especially good with autonomic symptoms), hydrotherapy, herbal supplementation such as Devils Claw, Cats Claw, Curcumin and Green Tee can all be useful in the management of this condition. Additionally, Arnica cream can also be used for bruising. Encouragement of non-weight bearing endurance activities such as swimming, and cycling to stimulate the endurance red muscle fibres over the ballistic white muscles fibres, since the latter are preferably used in this movement population. End of range movements are either avoided or done with care where stability is emphasised over mobility.
People frequently complain of subluxation and dislocating knee caps and shoulders whilst undertaking a spectrum of activities from sleeping to sporting endeavours. A good friend of mine, Brazilian Physiotherapist and Researcher, Dr Abrahao Baptista, has used muscle electrical stimulation on knees and shoulders to retrain the brain to enhance muscular cortical representation which reduce the incidence of subluxations and dislocations.
Abrahao wrote : "my daughter has a mild EDS III and used to dislocate her shoulder many times during sleeping. I tried many alternatives with her, including strengthening exercises and education to prevent bad postures before sleeping (e.g. positioning her arm over her head). What we found to really help her was electrostimulation of the supraspinatus and posterior deltoid. I followed the ideas of some works from Michael Ridding and others (Clinical Neurophysiology, 112, 1461-1469, 2001; Exp Brain Research, 143, 342-349 ,2002), which show that 30Hz electrostim, provoking mild muscle contractions for 45' leads to increased excitability of the muscle representation in the brain (at the primary motor cortex). Stimulation of the supraspinatus and deltoid is an old technique to hemiplegic painful shoulder, but used with a little different parameters. Previous studies showed that this type of stimulation increases brain excitability for 3 days, and so we used two times a week, for two weeks. After that, her dislocations improved a lot. It is important to note that, during stimulation, you have to clearly see the humerus head going up to the glenoid fossa"
Yoga vs Pilates
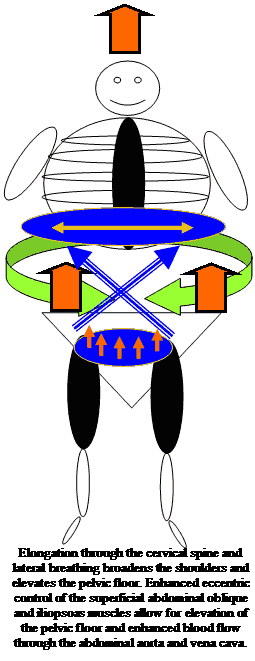
Many hyper-mobile people love yoga. They are good at it. However, they could be pushing themselves from a fine line of hyper-mobility to functional instability, pain and muscle spasms. The latter feeling of stiffness, drives them to do more yoga, ultimately perpetuating a vicious cycle which could ultimately end with chronic neurogenic pain. The reality is that hyper-flexible people should choose a more gentle form of yoga and consider a form which encourages stability. Other disciplines may be more appropriate such as Pilates or more specific stabilising physiotherapeutic exercises, involving isometric contractions, oscillations and balance. Alternatively, mind-body holistic approaches such as Feldenkreis and Alexander technique may be more appropriate. The mere elongation of the upper neck, in Alexander technique, activates the pelvic floor, deep core, diaphragm and shoulder blade stabilisers.
Marathon vs Sprinting
Comparing a marathon runner with a sprinter is like comparing an African Wild Dog with a Springbok. The former has the ability to run for days, whereas the latter has the fastest speed of any animal on earth.


You will very rarely find a 'floppy' lined up at the start of a marathon. They like to sprint and are frequently good at other ballistic activities such as high jump, pole volt, gymnastics. The 'stiffy' on the other hand loves the marathon as their stiffness stabilises them. Hence, 'floppies' need to stabilise. The stabilising muscles are the deepest layered ones, those which frequently only cross one joint and cannot easily be touched. Non-impact endurance exercise should therefore be encouraged. Sports such as swimming and cycling encapsulate this. However, even here, shoulder impingement needs to be avoided, whilst swimming (hydrotherapy), with good shoulder blade and core stability. Hydrotherapy conditioning can be practice out of water with a Swiss Ball and with Theraband exercises. Cyclists may develop knee, back and neck pain so they need to do a lot of gluteal and hamstring training in a closed kinetic chain e.g. reverse lunges for the knee, and should - shoulder blade - neck and back exercises for the upper body postures. Endurance exercise may also help calm the autonomic sympathetic nervous system, which is often seen as dysfunctional in people with EDS. Postural Orthostatic Tachycardia Syndrome (POTS) is frequently found amongst people with hypermobility. It is essentially an imbalance between heart rate and blood pressure which affects cardiac output (= SV x HR). The Modified Dallas POTS Exercise Program can be found here, which describes a progressive 4-6 month exercise program.
Rock climbers are frequently hypermobile people. Clinically, I've found hypermobile people prefer to pull rather than push. They are pulling energy in towards themselves creating a stabilising force. However, they seem, initially, to gain a lot from yoga, where a lot of pushing stabilisation work can occur in positions such as high plank, down-facing dog, etc. However, too much of a good thing can become a bad thing. Stabilisation, without the aim of gaining range of movement, but rather, controlling range of movement should be the objective. Muscle synergies can play a very important role, where a group of muscles from the legs to the arms can be stabilising, whilst one limb is moving, the others are dynamically or statically stabilising. The classic three points of contact in rock climbing. Interested readers should look at the climbing section of this website for further information. There are links to exercises, concepts of shoulder and shoulder blade-thorax stability, as well as hip-pelvic-back stability.

Agility vs Clumsiness and Deterministic Chaos
Hyper-mobile people tend to be either highly coordinated or clumsy. There doesn't appear to be a middle ground. I therefore like people to use exercises which either are isometric, pull energy towards them (pull up vs a push up), and use oscillations. These oscillations or periodicities are able to encourage movement around a fixed point based on visio-spatial (eyes), cerebro-vestibular (ears), and musculoskeletal inflection points. These inflection points can be the therapeutic building block of all movements. It needs to be remembered that when the (chronically) injured person comes to you, if they once were a 'great' athlete (which is very common), they had learnt to move outside of the 'average' movement system. Their brains are still tuned to those fundamentals, but are now over-ridden by the 'static' of pain generator input! Those movement patterns of a prior pre-injured life are still somewhere to be found. Like peeling back the layers of an onion to disseminate what is what, and the rebuilding the system. However, it should be remembered, that those movement patterns were born of fast controlled->uncontrolled movement. These 'outliers' are essentially what 'deterministic chaos' encapsulates.

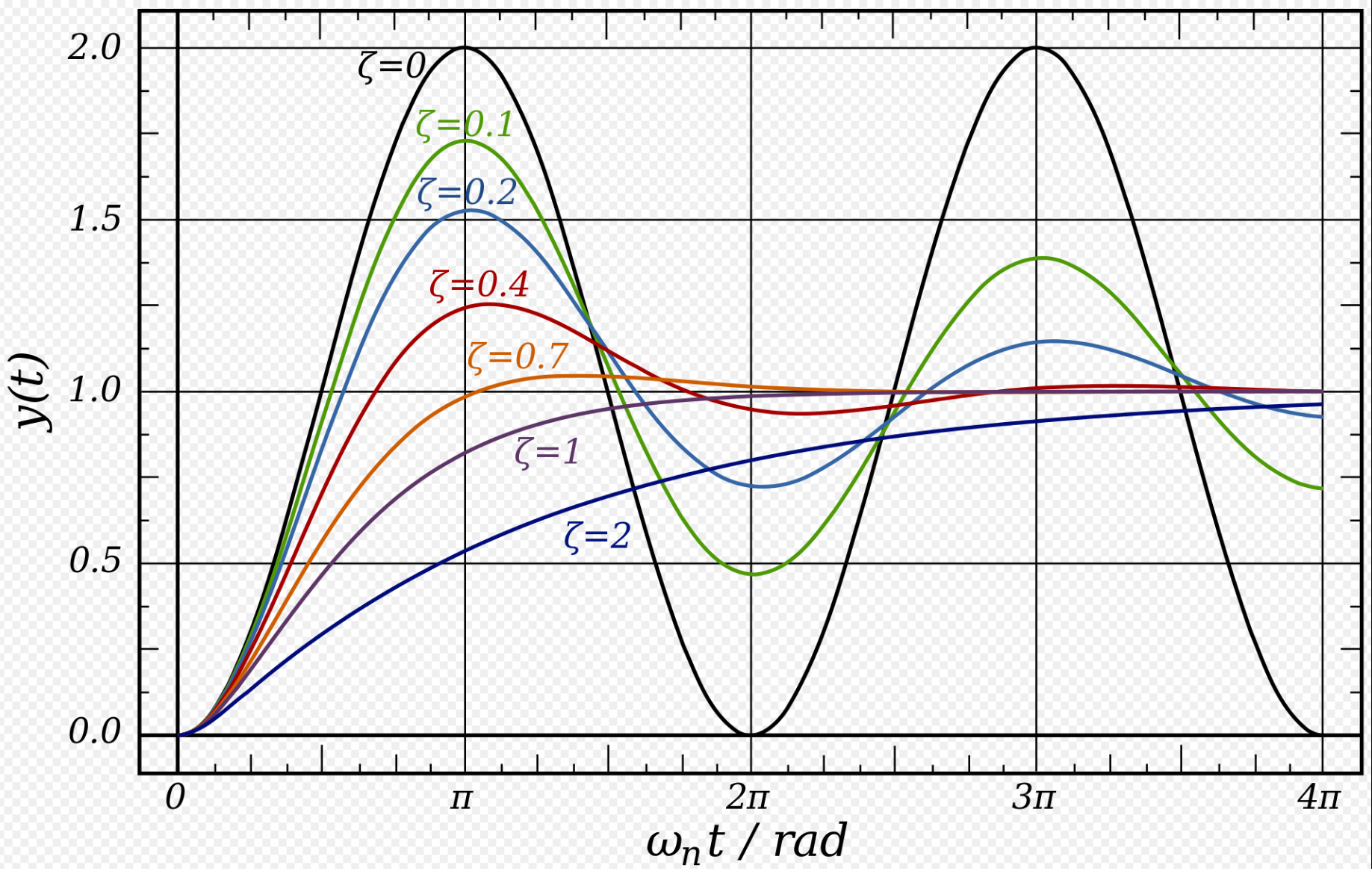
Ultimately, only oscillatory balancing movements, based on a solid isometric gluteal base, can achieve achieve redemption. Activation of gluteal muscles results in the activation of the core, not vice versa!!!! Activation of the gluteal muscles also improves arm strength.
Exercises - draw energy into the body to stabilise
People need to use their muscle synergies to support the skeletal structures, not the other way round. Muscles support bones and organs, bones don't support muscles, they act as levers for the muscles. Consider the body to be lying in 'slings of muscles', similar to when you lie in a hammock. These slings are known as the front/anterior, back/posterior (x's 2, 3, 4, 5 and 8), inside/medial and outside/lateral (x's 1 and 6), as well as spiral slings. The following exercises are designed to invoke the muscle bellies in the loading mechanism. The strain should be felt within them, not at the joints. The joints are just the axels around which movement occurs. Basically, hyperflexible people should avoid the tendency to hyperextend/flex their joints, and nullify the habit of overloading their tendon, ligament and joint surfaces.
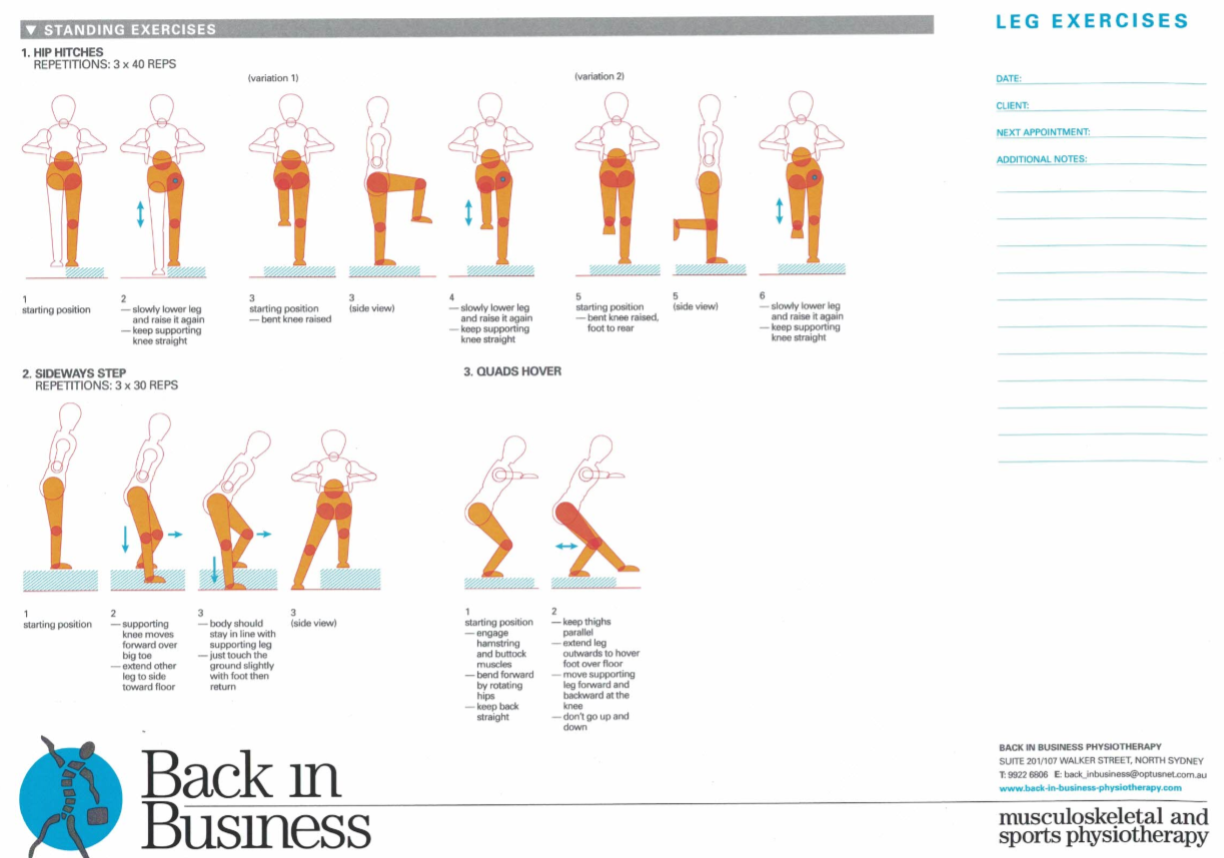
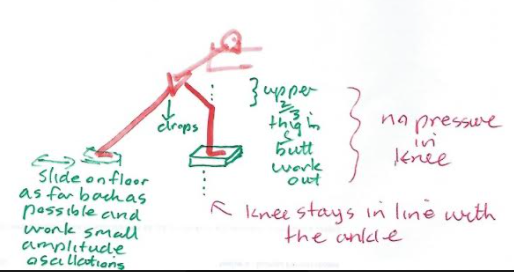
In X's 2 try to go back and diagonally back whilst keeping the knee over the ankle and dropping the stance hip down. There should be no pressure in the knee. All the pressure should be in the butt, hamstrings and quads in the upper 2/3rds of the thigh. Similarly in X's 3 lean forward enough so that you experience the butt, upper quads and hammies doing the work, with no pressure in the knee.
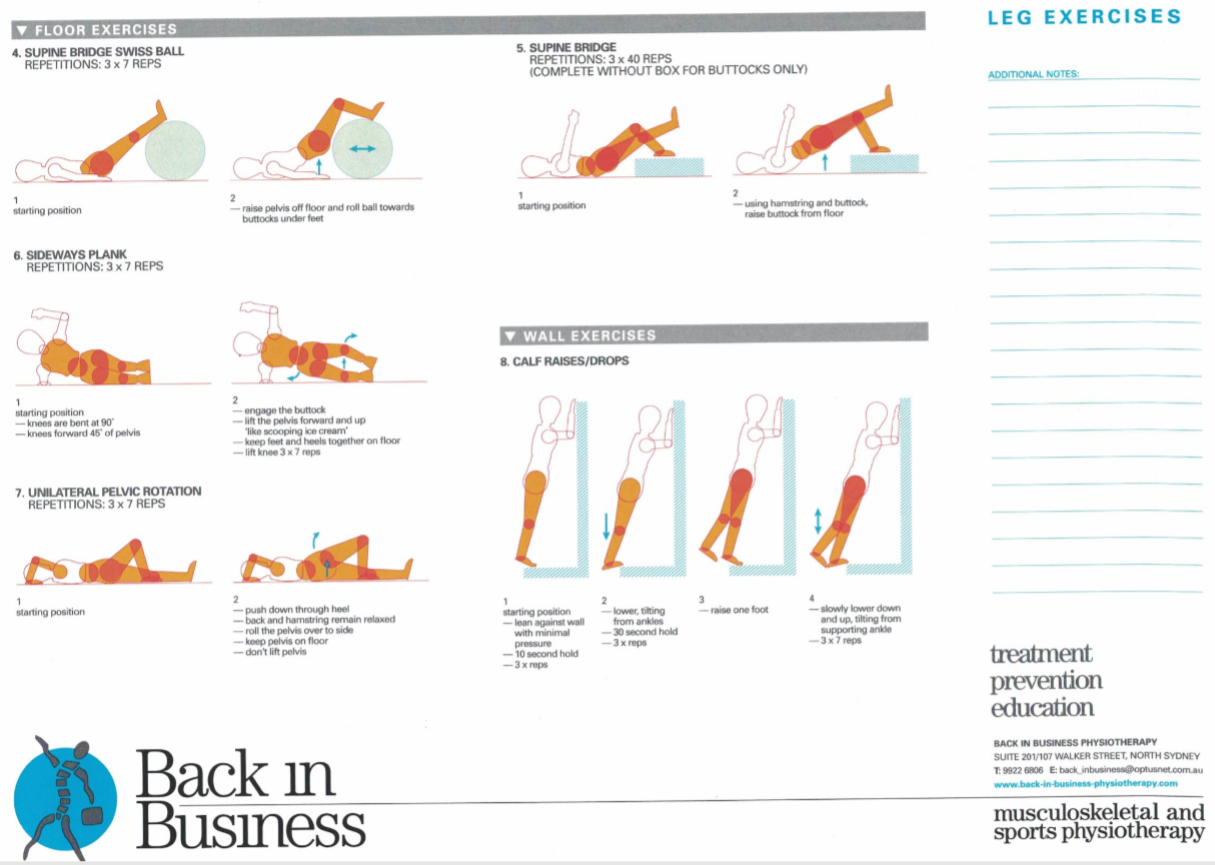
Back X's - posterior sling : 7, anterior - posterior sling : 6, spiral : 7, medial and lateral and anterior : 11 (add Buttock clenches and you get posterior as well)
Spiral : 12, 13 and 15, Lateral and Posterior : 14, Anterior : 17 Medial : 22, Anterior : 20, Posterior : 21
Shoulder Blade stabilisers
Immune system
People with hypermobility may also have an auto-immune disorder. Ironically, some hyper-mobile children develop severe stiffness later in life as a result of sero-negative arthropathies such as Ankylosing Spondylitis and Psoaratic Arthritis. The latter frequently is associated with scaly inflamed skin. Additionally, irritable bowel syndrome may also occur. The gut is known to be essential to immune health, where an imbalance can lead to several dysfunctional immune-inflammatory interactions.
See : Trends in Microbiology, Moya and Ferrer: “Functional Redundancy-Induced Stability of Gut Microbiota Subjected to Disturbance” http://dx.doi.org/10.1016/j.tim.2016.02.002
Additionally, energy species of the gut interact with skeletal muscle. Skeletal muscles, not only allow us to perform movement and work, they are also an important immune endocrine organ.
Surgery :
The effect of surgical intervention has been shown to be favourable in only a limited percentage of patients (33.9% Rombaut et al 2011, Arch Phys Med Rehab, 92, 1106-1112). Three basic problems arise. First, tissues are less robust; Second, blood vessel fragility can cause technical problems in wound closure; Third, healing is often delayed and may remain incomplete.
Voluntary Posterior Shoulder Subluxation : Clinical Presentation
A 27 year old male presented with a history of posterior shoulder weakness, characterised by severe fatigue and heaviness when 'working out' at the gym. His usual routine was one which involved sets of 15 repetitions, hence endurance oriented rather than power oriented. He described major problems when trying to execute bench presses and Japanese style push ups.
In a comprehensive review of 300 articles on shoulder instability, Heller et al. (Heller, K. D., J. Forst, R. Forst, and B. Cohen. Posterior dislocation of the shoulder: recommendations for a classification. Arch. Orthop. Trauma Surg. 113:228-231, 1994) concluded that posterior dislocation constitutes only 2.1% of all shoulder dislocations. The differential diagnosis in patients with posterior instability of the shoulder includes traumatic posterior instability, atraumatic posterior instability, voluntary posterior instability, and posterior instability associated with multidirectional instability. Laxity testing was performed with a posterior draw sign. The laxity was graded with a modified Hawkins scale : grade I, humeral head displacement that locks out beyond the glenoid rim; grade II, humeral displacement that is over the glenoid rim but is easily reducible; and grade III, humeral head displacement that locks out beyond the glenoid rim. This client had grade III laxity in both shoulders. A sulcus sign test was performed on both shoulders and graded to commonly accepted grading scales: grade I, a depression <1cm: grade 2, between 1.5 and 2cm; and grade 3, a depression > 2cm. The client had a grade 3 sulcus sign bilaterally regardless if the arm was in neutral or external rotation. The client met the criteria of Carter and Wilkinson for generalized liagmentous laxity by exhibiting hyperextension of both elbows > 10º, genu recurvatum of both knees > 19º, and the ability to touch his thumb to his forearm
Headaches
Jacome (1999, Cephalagia, 19, 791-796) reported that migraine headaches occurred in 11/18 patients with EDS. Hakim et al (2004, Rheumatology, 43, 1194-1195) found 40% of 170 patients with EDS-HT/JHS had previously been diagnosed with migraine compared with 20% of the control population. in addition, the frequency of migraine attacks was 1.7 times increased and the headache related disability was 3.0 times greater in migraineurs with EDS-HT/JHS as compared to controls with migraine (Bendick et al 2011, Cephalgia, 31, 603-613).
People suffering from soft tissue hypermobility, connective tissue disorder, Marfans Syndrome, and Ehler Danlos syndrome may be predisposed to upper cervical spine instability. Dural laxity, vascular irregularities and ligamentous laxity with or without Arnold Chiari Malformations may be accompanied by symptoms of intracranial hypotension, POTS (postural orthostatic tachycardia syndrome), dysautonomia, suboccipital "Coat Hanger" headaches (Martin & Neilson 2014 Headaches, September, 1403-1411). Scoliosis and spondylolisthesis occurs in 63% and 6-15% of patients with Marfans syndrome respectively (Sponseller et al 1995, JBJS Am, 77, 867-876). These manifestations need to be borne in mind as not all upper cervical spine instabilities are the result of trauma. Clinically, serious neurological complications can arise in the presence of upper cervical spine instability, including a stroke or even death. Additionally, vertebral artery and even carotid artery dissections have been reported during and after chiropractic manipulation. Added caution may be needed after Whiplash type injuries. The clinician needs to be aware of this possibility in the presence of these symptoms, assess upper cervical joint hypermobility with manual therapy techniques and treat appropriately, including exercises to improve the control of musculature around the cervical and thoracic spine. Atlanto-axial instability can be diagnosed by flexion/extension X-rays or MRI's, but is best evaluated by using rotational 3D CT scanning. Surgical intervention is sometimes necessary.
Concussion
Severity of concussion has been associated with JHS. An interesting case of EDS and it's affect on post concussion syndrome can be read elsewhere on this site.
Temperomandibular Joint (TMJ) Disorders
The prevalence of TMJ disorders have been reported to be as high as 80% in people with JHD (Kavucu et al 2006, Rheum Int., 26, 257-260). Joint clicking of the TMJ was 1.7 times more likely in JHD than in controls (Hirsch et al 2008, Eur J Oral Sci, 116, 525-539). Headaches associated with TMJ disorders tend to be in the temporal/masseter (side of head) region. TMJ issues increase in prevalence in the presence of both migraine and chronic daily headache (Goncalves et al 2011, Clin J Pain, 27, 611-615). I've treated a colleague who spontaneously dislocated her jaw whilst yawning at work one morning. stressful for me and her! Generally, people with JHD have increased jaw opening (>40mm from upper to lower incisors).
Conclusion
EDS and JHS are complex, multi-factorial debilitating conditions, which frequently, for many years, are misdiagnosed. Therapeutic intervention will depend upon the stage, stability, irritability and severity of the disease, Issues such as misuse, abuse, overuse and disuse will also need to be entertained. Regardless, a multi-modal approach to a multidimensional problem needs to be considered. Importantly, the individual must be engaged in every stage of the treatment intervention process.
Updated 28 October 2022