Chronic Low Back Pain
Martin Krause, B.App.Sci (Physio), Master Appl Science (Manipulative Physio), Grad Dip Hlth Sci (Ex and Sport), Grad Cert Hlth Sc Edu
At Back in Business Physiotherapy we treat people with passion and care, as we know that your chronic back pain can likened to being a prisoner inside your own body. We take an holistic approach whereby we examine the cause of chronicity and the multiple inter-relating aspects of musculoskeletal dysfunction in the body, which can be the source of continued pain generating mechanisms.
Interestingly, the transition from acute to chronic pain occurs during the acute phase of injury. The brains' reaction to injury is dependent upon it's previous experiences of injury, pain and recovery. Therefore, the perceived threat to the persons integrity, by the trauma, will directly affect the ultimate outcome. During the acute phase of injury, people generally react by avoiding the painful or injurious movement. Yet as the problem becomes chronic they tend to make movements which actually aggravate the painful condition. It is almost as if the person has had such an intense relationship with their problem that they now sympathise with it, move to it's beat and act in a similar way to the "Stockholm syndrome" whereby the kidnapped sympathise with the kidnappers.
Another explanation can be the re-allocation of cortical processing to a new 'locus of control', which employs redundant systems. Using a Bernsteins locus of control perspective, movement occurs around a 'fixed point'. Such a fixed point may be a simple synergy around a given joint, or a complex of synergies involving various muscle slings. The simplest empirical formula would be based on Hooke's Law of a mass oscillating on a spring. The greater the perturbation from the centre, the greater the 'damping mechanism' of the spring. In the case of human biology, the 'spring' represents total muscle tone around a joint or movement complex. Game theory would suggest that, rather than examine muscles as agonists and antagonists, nett gain is represented by optimal synergy, In the case of chronic pain, some muscles may be atrophied from disuse, others hypertrophied from overuse, whilst other muscles might be in spasm. Typically, the deep endurance stabilising slow twitch muscles reduce their activity, fast twitch muscles twitch faster for less time and thereby still atrophy, whilst the brain representation of key muscles which are supposed to be the prime mover or vector, either reduce or are represented in a different part of the cortex. The somatosensory and motor focus changes to pain related feedback rather than objective related control. Is this why, when we bump our elbows badly, we bump them again and again, until at some given time we stop bumping it?
If movement control is based on linear mechanics, oscillations and temporal factors, what if we took a non-linear 'deterministic chaos' approach to oscillations and locus of control? We've heard of the the Butterfly Effect and the flapping of it's wings creating a hurricane on the other side of the planet. What if it's the inverse, those beating wings calm the hurricane? Oscillations in one part of the body redefine oscillations in the affected region of the body. Oscillatory movements have been employed by Musculoskeletal Physiotherapists, trained in the Maitland technique, for many decades, to reduce muscle spams. Exercises of oscillations (in for example the shoulder) can influence oscillations elsewhere in the body (in this case the low back on the opposite side). Similarly, oscillatory joint mobilisations in one part of the body (cervical spine and lumbar spine) can affect muscle spasms/tension elsewhere in the body (limbs).
Some of the more profound oscillatory effects can occur in the thorax. This shouldn't be surprising as breathing normally occurs in some form of rhythm. Moreover, the transient changes in the rhythm, through exertion, is an important aspect for establishing the median, as it provides an outlier, on which to base the damping mechanism. Joint mobilisations of the lower three ribs have significant impact on lateral thigh tightness. Thoracic ring relocation techniques improves the biomechanics of the thorax and probably influences sympathetic nervous system function. Importantly, thoracic rotation influences gluteal muscle activation, whereby rotation in one direction is countered at end of range by gluteal activation on the side opposite to the rotation. Gluteal activation has a profound influence on core stability. Importantly, activation of the core muscles doesn't activate the gluteal muscles, BUT gluteal activation does activate the core muscles. Simple ring relocations can immediately influence active SLR and gluteal activation of leg extension.
An intriguing concept, oscillations in another part of the body can be used to establish harmonic frequency elsewhere. For example, arm movements activating the opposite erector spinae activity, pelvic oscillations for scapular control, arm lifts for contra-lateral gluteal activity.
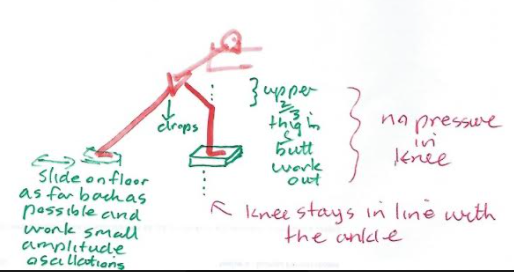
Alternate kneading of the hands into something soft activates the abdominal muscles, spinal rotators and scapula muscles. Oscillations of the pelvis around the hip activates eccentric scapula control.
Alternate lifting of the arm off the wall activates the opposite buttock muscle.whilst stretching the opposite calf
Alternating arm flexion/extension around the 90 degree angle activates the opposite erector spinae muscles of the low thorax and upper lumbar spine. Moving through the horizontal with a consistent oscillation also has varying effects on those muscles.
Please read on for more precise scientific (beyond mechanical) and clinical detail : https://www.back-in-business-physiotherapy.com/health-advocacy/exercise-and-the-immune-system-during-covid-19.html.found elsewhere on this website
Low back pain can be chronic for several reasons. In some instances, it's because the extent of examination and the scope of treatment wasn't adequate. In other cases, the neuropathic nature of nerve injury, create instances whereby normal mechanical input is 'misread' and amplified by the nervous system. In other cases, the mental health of the person is profoundly affected by pain, which in turn has a vicious cycle of self-perpetuation. Physiotherapists, dealing with the movement system, need to bear in mind the multi-dimensional nature of chronic pain.
The following describes the multiple dimensions of chronic pain and the ways clinicians and clients can analyse and differentiate various aspects. Ultimately, as clinicians we need to peel away the onion, layer by layer, to get to the crux of the matter, and then rebuild, step by step, the jig saw puzzle, into a meaningful clinical strategy, employing all the knowns and recognising the unknowns. placing a value for each, whilst maintaining a realistic context of inflection points, representing functional outcomes, as well as limitations.
Index
Cycling versus specific exercise
Anticipation of Pain - placebo/nocebo effect
Forebrain mechanisms of nociception
Role of 'values' in a contextual behavioural setting
Treatment and reduction in catastrophizing
Socratic Questioning and Allostasis
Treatment techniques for central programming errors
Non Specific Low Back Pain and Peter O'Sullivan approach to classification
Neuropathic and neurogenic pain cycle
Do you remember how much you used to have to concentrate when you learnt to drive? Eventually, the task became automated and effortless. However, what happens when you are in an unfamiliar area, you need to look at a map, there is lots of traffic and the mobile phone rings because you are running late for the meeting that you have to chair? Your cognitive systems are bombarded with competing information trying to make itself the priority in your limited processing systems. Similar to RAM in those old computers which couldn't keep up with newer and better software programmes, everything starts to slow and grind to a halt.
Back pain can have similar effects on your processing capacity. Reduced variability of postural strategies has been considered to prevent normalization of motor strategies induced by low back pain (Moseley & Hodges 2006). Together with a 'viscious cycle' of nociceptive input,and altered muscle spindle proprioceptive input as well as a motor derived pain adaptation can create considerable input-output ambiguity within the nervous system (Madelaine 2008). With constant cognitive hyper-vigilance, a person in pain can have their RAM slow because they have less redundancy to cope with new stimuli. The glutamate-NMDA receptors of the prefrontal cortex and noradrenergic receptors of the locus coereleus may be viewed as the RAM of pain processing. The locus coereleus in particular has been considered an integrator of cerebral activity, helping maintain 'neural synchrony' like a conductor of an orchestra. However these nuclei can undergo neurocytotoxic effects in the presence of excessive and ambiguous interoceptive and exteroceptive inputs. This, may reduce the ability to cope with fear and anxiety in the amygdala and limbic systems. Furthermore, the anterior cingulate cortex (ACC) with its connections to the hippocampus may have it's memory for pain and disability amplified. This is significant as the ACC is active in 'anticipation' of noxious stimuli (see figure by Koyama below). Connections with the hypothalamic-pituitary axis can result in hormonal imbalance. It is probable that interoceptive bombardment of the CNS by inflamed peripheral nociceptors may be reduced through musculoskeletal physiotherapy hands-on techniques designed to reduce pain and muscle spasm. However, more frequently after the initial injury no inflammation exists and hence to prevent chronicity, clear explanations by the physiotherapist and structured goal oriented exercise regimes are used to help the person filter ambiguous intero and extero-ceptive information, thereby adding clarity to 'feed-forward' anticipatory mechanisms. Never-the-less muscle imbalance and atrophy due to inactivity as a result of 'fear-avoidance' behaviour can be addressed using specific exercises for the anti-gravity endurance stabilising muscles, whilst addressing co-ordination of the global mobilising muscles. Such an activity programme of specifc exercises must be accompanied by a desensitization process of graded exposure to 'fearful' activities. Hereby, hypervigilance and excessive hormonal stress responses (such as the release of adrenaline and cortisol) to 'perceived threats' is reduced. Thus, cortical 'clarity' is obtained whereby clients will often makes comments such as " the cloudiness has lifted from my brain" or "that they have awakened from a bad dream"

Moseley et al (2001 Abstracts - Society for Neuroscience) used attentional demands such as the stroop test to examine motor control and pain. They found that it was the fear of pain rather than the attention-demanding nature of pain which could partially explain changes in motor control. Fear connotes an identifiable threat (eg King Brown snake), whereas anxiety connotes the possibility of threat. Fear-avoidance relates to the behaviour that an identified activity may have (real or imaginary). Kinesiophobia refers to the patient experiencing "an excessive, irrational, and debilitating fear of physical movement and activity resulting from a feeling of vulnerability to painful injury or reinjury" (Kori SH et al Pain Management 1990; Jan/Feb:35 to 43)

A persons initial reaction to an injury is usually one of shock. This is generally followed by a self appraisal of the situation "can I cope with this?", "do I have a strategy to cope with this?" If the answer is 'yes' then the normal process of recovery (in 90% of the population) within 6 weeks takes place. If the answer is 'no' then panic may set in and a process of 'catastrophizing' and 'rumination' begins. The latter strategy leads to 'activity avoidance' behaviour and desperate search for answers. Even at this stage, this can be an 'adaptive' process whereby the person seeks and finds the answers with the aid of a health professional and develops a active strategy for recovery. However, this becomes 'mal-adpative' when a passive coping strategy is enlisted which leads to 'learned helplessness'. Generally, a past history of 'passive coping' strategies can be gleaned on questionning. Some people who have had multiple painful procedures as children (e.g. premature baby) learn that active escape from pain was impossible. Generally, people in chronic pain will have also enlisted the help of mutiple practitoners, as well as used the internet to find an explanation for the 'unexplained chronicity' of their pain.
Greater exposure to past traumatic life events and depressed mood were most predictive of chronic pain whilst depressed mood and negative pain beliefs were most predictive of chronic disability. More cummulative traumatic events, higher levels of depression in the eraly stages of a new pain episode, and early beliefs that pain may be permanent significantly contributed to increased severity of subsequent pain and disability (Young Casey et al 2008, Pain, 134, 69 to 79)
Avoidance behaviours occur in anticipation of pain and generally persist because there are few opportunities to correct the eroneous expectations which drive them. This has a deliterious effect in the engagement of ADL which then in turn can lead to mood disturbances, irritability, frustration and depression. The fear-avoidance behaviour leads to secondary consequences of deconditioning whereby even normal activity such as walking, stair climbing or carrying the shopping leads to excessive fatigue, heart palpitations, nausea and distress.

Education and reassurance
Simply reassuring a person suffering pain can be seen as a lack of understanding of the legitimacy of their complaint. Even a series of positive results such as MR imaging can decrease a patients reported well-being (LInton et al 2008, Pain, 134, 5 to 8). Moreover, educating a client to the pain matrix or virtual pain brain can have its limitations if it isn't experience-based in its methodology. Cognitive, emotional, and behavioural factors have a combined impact on the effect of reassurance. Acknowledging and understanding what the patient is experiencing includes elements of respect and acceptance which reflects the practitioners use of empathy when dealing with the multiple impacts that pain is having on a persons life. This in turn may influence their fear and worry which should result in more positive impact on avoidance behaviour patterns (Linton et al 2008, Pain, 134, 5 to 8). Interested readers should also review the Explain Pain Book by Lorimer Moseley and David Butler (NOI Publications, Adelaide, Australia)
Education and Constructivism
Constructivism describes the process of learning and acquiring knowledge through experiential reasoning. The assumption underlying 'constructivism' is that we are 'life long learners' (3 l's) and that each and every clinical encounter allows a unique opportunity to learn, relearn and refine as well as reorganise and restructure the knowledge base. Furthermore, constructivist theory suggests that learning occurs which is based on each individuals unique prior experiences. Truth is considered relative to the individuals construct and hence diverges from logical positivism of science where 'truth' can exist alone without reference to the observers perceptions. This is similar to scientific philosophy of 'relative truths' or the 'relativity of knowledge' espoused by Feyerabend (1975), Kuhn (1970), Popper (1963). All of us would agree that science isn't just a collection of laws, or a catalogue of unrelated facts. Rather, it is a creation of the human mind relating to making sense of the world. Hence, in musculoskeletal physiotherapy we must endeavour to match the science with our clinical reasoning which should make sense to the individual or organisations with whom we are interacting.
Candy (1991, p 263) states that "the constructivist perspective differs significantly from the view of knowledge as deriving from a process of copying or replicating." Hence, "we know reality only by acting on it.....The active interaction between the individual and the environment is mediated by the cognitive structures of the individual......and what we learn from the environment is dependent upon our own structuring of those experiences." (Nystedt and Magnusson 1982, p34)
People who are suffering from chronic low back pain need to be engaged in education by being included in the dialogue of the clinical reasoning process. The person suffering chronic pain needs to be able to suspend or alter beliefs if perceptions are to be changed. Changes in perceptions allow the opportunity for the construction of a new movement reality. Therefore, the therapist needs to ascertain what the clients values and beliefs are and how these impact on the clients life.
Beliefs and Avoidance
Pain caused by length differences in legs -> avoidance of running and squatting
Pain caused by spine 'worn out' and back bones ' pressed together' pain warning signal to stop -> avoidance of heavy lifting, painting and craft, jogging
Pain caused by 'no cartilage between the 5th and 6th lumbar vertebrae leading to bone pressing on nerves' -> avoidance of vacuum cleaning, shopping, cleaning windows
Pain caused by 'crack in arch of one of my back bones' and 'inflammation in muscles' -> avoidance of rotating body, heavy manual labour, hroseback riding, bending forward
Pain is caused by my scoliosis and leg length difference -> avoidance of wiping floor, making bed, vacuum cleaning, bending foward
(Boersma et al 2004, Pain, 108, 8 to 16)
Cycling versus specific exercise for chronic low back pain
Sixty-four patients with low back pain were randomly assigned to 8 weeks of specific trunk exercise group (SEG), or stationary cycling group (CEG). Self-rated pain, disability, catastrophizing and FAB scores were collected before, immediately after (8 wk), and 6 months after the training program. Clinically meaningful improvements were defined as greater than a 30% reduction from baseline in pain and disability scores. At 8 weeks, disability was significantly lower in the SEG compared with the CEG (d = 0.62, P = 0.018). Pain was reduced from baseline in both the groups after training (P < 0.05), but was lower for the SEG (P < 0.05). FAB scores were reduced in the SEG at 8 weeks, and in the CEG at 6 months. No between-group differences in Fear Avoidance Beliefs (FAB) scores were observed. Similar reductions in catastrophizing in each group were observed at each time point. At 6 months, the overall data pattern suggested no long-term difference between groups. Hence, long term bicycle riding can play a significent role in the reduction of the severe behavioural affects of chronic low back pain. (Marshall PW, Kennedy S, Brooks C, Lonsdale C. (2013) Pilates exercise or stationary cycling for chronic nonspecific low back pain: does it matter? a randomized controlled trial with 6-month follow-up.Spine;38(15):E952-9)
Cortical Plasticity
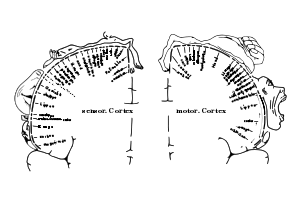
The motor and sensory hormonculus describes use dependent and bilateral representation of peripheral receptive fields in the cortex
Changes in cortical representation after deafferentation damage ot a peripheral nerve
Cortical reorganisation after training
Pain and altered movement behaviour are likely to alter the somatotopic representations in the brain. This is probably because pain redefines percepetion and perception redefines the meaning of pain, thereby altering the weighting and meaning of peripheral sensory inputs. Expectations become blurred which reduces the capacity of the fine filtering mechanisms. The good news is that it may be possible to alter the somatotopic representation back again with appropriate therapy and training.
Areas of the brain associated with pain processing
- Hippocampus & Amygdala
Pain activation of the Amygdala and Hippocampus were first shown by Hsei et al (1995). The Amygdala has an intimate involvement with 'fear avoidance' behaviour. The Hippocampus does not have a direct involvement in pain processing, however it is involved with the consolidation of long term memories (Zola-Morgan et al 1989). In particular, hippocampal damage inhibits the assimilation of contextual information preventing animals solving tasks that require the use of mapping strategies or from responding to contextual cues indicating danger (Morris et al 1982). Several neuroanatomical studies have shown that the ACC receives substantial input from the amygdala (Price 1984, Vogt et al 1987). Additionally, there are widespread hippocampocortical connections with the orbitofrontal cortex, ACC and the PHG (Van Hosen et al 1993). The connections between the ACC, insula and amygdala-hippocampal-prefrontal circuits consititute a network within which fear and contextual information relevant to pain can be integrated (Derbyshire et al 1997, Pain, 73, 431 to 445)
- Anterior Cingulate Cortex
The midcingulate is likely to be involved in functions relating to motor response and has been implicated in response selection during divided attention tasks (Pardo et al 1990, orbetta et al 1991, Bench et al 1992). Processes associated with affective emotional content are liable to involve the perigenual cingulate region, where electrical stimualtion of this region can evoke 'fear' and other emotional responses (Bancaud & Talairach 1992). Additioanlly, this area has been shown to be activated in PET scans when recalling 'sad' events (George et al 1995).
-Thalamus
The medial pain system project to structures such as the ACC, Insular and Prefrontal Cortex and may be involved in the motivational-affective features of noxious stimuli, whereas the lateral pain system which incorporates the VPL projects to the somatosensory cortex and is likely to bew involved in sensory-discriminative aspects of noxious stimuli (Derbyshire et al 1997, Pain, 73, 431 to 445).
- Insula
The insula connects reciprocally with somatosensory II (S2), receives input from spinothalamically activated posterior thalamic nuclei and projects to the amygdala and perirhinal cortex (Firedman & Murray 1986), which makes it well suited for the integration of information related to the affective and reactive components of pain (Coghill et al 1994, Hsieh et al 1995). Activation of the anterior insular arises due to the anticipation of pain, whereas the posterior insular is activated during the actual experience of pain (Ogino et al 2007, Cerebral Cortex, 17, 1139 to 1146)
- Prefrontal cortex and inferior parietal cortex
In general the prefrontal cortex is involved with planning involving the behavioural and attentional organisation during pain (Derbyshire et al 1997, Pain, 73, 431 to 445, Hsieh et al 1995, 1996). The PFC is therefore associated with 'vigilance'. Neuroanatomical studies suggest that the DLPF cortex works closely with the posterior parietal cortex (PPC). When considering the attentional systems of the brain, these can be conceptualised into the anterior focal attention system and the posterior preconscious orientation (Possner & Rothbart 1991)
- The lateral Premotor Cortex
Loss of premotor cortex impairs the ability to develop an appropriate strategy for movement. It receives its input principally from the posterior parietal cortex (PPC) and from thalamic neurones relaying information from the globus pallidus
- The somatosensory cortex (S1)
Probably involved in the sensory-discriminative aspects of pain processing. Sensory discriminative training for phantom limb pain (Flor et al 2001, Lancet357(9270), 1763 - 4), and tactile discrimination training for complex regional pain syndrome (Mosely & Wiech 2008, Pain), both target body maps in the primary somatosensory cortex and both show a clear increase in tactile acuity, which is a marker of primary somatosensory cortex organisation and decreased pain (Moseley 2008 Manual Therapy, 475 to 477). Moseley (2008) speculated that it may be these body maps which hold the key as to why some patients respond better to comprehensive examination than they do to treatment.
Apkarian et al (2005) referred to 'pain matrx' consisting of the dorsolateral prefrontal, insular, anterior cingulate, primary and secondary sensory cortices and the thalamus.
The medial pain system has been implicated during tactile stimulation with 'imagined allodynia'. Kraemer et al (2008) demonstrated activation of the ACC and bilateral activation of secondary somatosensory cortex (S2), insular cortex and prefrontal cortices in people experienced in allodynia who imagined their pain intensity (J Pain 9(6), 543 to 51). These results were replicated by Ogino et al (2007), where people viewed images of painful events and were told to imagine their pain. Additional to the areas mentioned, these investigators also found activation of the amygdala which may be associated with fear, and the activation of posteror parietal which may be associated with self-body centred co-ordinates. Activation of S2 was considered to be associated with the cognitive evaluative aspects of pain (Cerebral Cortex, 17, 1139 to 1146).
Investigations into brain function have demonstrated neuroplasticity including multiple changes seen on PET and fMRI. Although fMRI can now delineate areas (voxels) smaller than 1mm3, this area contains about 25000 neurones and 200 trillion synapses. Never-the-less changes seen include
- map expansion
- sensory reassignment (eg visual to auditory)
- compensatory masquerades
- mirror region takeover
Multiple studies indicate that activity in the mPFC and DLPFC are inversely related (Mayberg et al 1999, Northoff et al 2000). Moreover, Apkarian et al (2004) demonstrated that DLPFC gray matter density is decreased in chronic back pain. Together, mPFC activity reflects intensity of chronic back pain which is likely to be enhanced by DLPFC atrophy. The mPFC is also involved in emotions, response conflict and detection of unfavorable outcomes. Emotional reasoning enhances mPFC whilst depressing DLPFC. Since the DLPFC is involved with working memory, this may have implications for cognitive function such as emotional decision making (Apkarian et al 2004; Bailiki et al 2006, J Neuroscience, 26, 47, 12165 to 12173)
Both mental and physical trauma resulting in chronic pain affects higher centre processing of sensory information which in turn affects motor and hormonal responses. Concepts of brain neuroplasticity can be used by the practitioner in a positive manner to ameliorate mal-adpative changes to which the brain may have undergone (Doidge N 2007, The Brain That Changes Itself, Viking Penguine publications).
see Pain in the Brain for imaging
Cognitive behavioural therapy (CBT)
Cognitive behavioural therapy (CBT) focuses on the content of the disorder which has lead to the excessive behaviour. Through progressive cognitive appraisal and re-appraisal the irratitionality of the behaviour is reduced. Another method of dealing with mal-adaptive behaviour is to recognise the behaviour for what it is and attempt to associate this behaviour with positive thoughts, experiences and activities. Hereby, neurons that fire together, wire together into a positive movement experience. The original fear & anxiety may not be extinguished but the ability 'to move on' and the ability to neither dwell on the anxiety nor on the content of that anxiety is taught and learned. Importantly, education into how the brain processes and deals with information, using PET scans, fMRI's, flow diagrams, etc become very useful tools when explaining the usefulness of graded motor imaging (GMI) tasks. Recently, however, Lorrimer Moseley has suggested to firstly use computer generated images to distinguish any signs of cortical laterality bias either towards or away from the affected region. This appears to be particularly useful for CRPS, frozen shoulder and neuropathic limb pain, but may not be so relevant to spinal pain. Never-the-less, recognition and education of the problem are paramount to successful outcome.
Hsieh et al (1995)
click on image for greater resolution
"Living in the past is dwelling upon what cannot be changed, living in the future is creating the milieu for fear and anxiety, living in the now is the right environment for action and change"
Anticipation of pain affects the subjective experience of pain where expectations become reality
Treatment success and understanding the clients needs and preceptions can result in positive outcomes. In contrast, failed treatment or unrealistic expectations, unrealistic timeframes and undefined, poorly conceived goal setting may result in the 'nocebo' effect.


Placebo Response
Our subjective sensory experiences are thought to be heavily shaped by intereactions between expectations and incoming sensory information. Koyama et al (2005) found that as the magnitude of the expected pain increased, activation increased in the thalamus, insula, prefontal cortex, anterior cingulate cortex (ACC). However, when the expected pain was manipulated, the expectations of reduced pain powerfully reduced both the subjective experience of pain and activation of pain-related regions such as the primary and secondary somatosensory cortex (SI, SII), insular cortex, pre frontal cortex (PFC), mPFC (Raij et al 2005, PNAS, 102, 6, 2147 to 2151), ACC and cerebellum (PNAS, 102, 12950 to 12955)
Pain modulation by placebo have shown brain activations in the rostral anterior cingulate (rACC), insula, thalamus and mid-brain regions. During reduced pain expectation, increased acticvity in the orbitofrontal cortex (OFC) and dorsolateral prefrontal cortex (DLPFC) were seen (Watson et al 2009 Pain, 145, 24-30). Anticipation of pain reduction during placebo conditioning and post-conditioning activated fronto-cingulate structures included Prefrontal Cortex (PFC) structures DLPFC and MFC, anterior mid cingulate cortex (aMCC) and the dorsal posterior cingulate cortex (dPCC). The PCC is involved in visuospatial orientation and assessment of self-relevant sensation and the more dorsal PCC is associated with orientation of the body to both innocuous and noxious somtosensory stimuli, which combined are essential for the process of learning. Modulation of activity in the MCC has been associated with affective aspects of pain and pain intensity coding. The anticipation of reduced pain and actual perception of reduced pain could serve as the foundation of a self-reinforcing feedback loop underpinned by the previously associated learning (Watson et al 2009). Furthermore, for a placebo to be effective the memory of the effectiveness of a treatment developed during the learning conditioning phase must be retrieved and matched with the incoming sensory information, where the PFC with its role in memory retrievel and working memory plays an important part (Watson et al 2009).
All of these cerebral cortical areas receiving nociceptive informaton can be readily modulated by expectation-induced information. Because expectations are future predictions derived from both past experience and present context, this flow of expectation-related information may be crucial for the development of a 'perceptual set' . Given the highly distributed and parallel nature of pain processing, the 'perceptual set' needs to be a highly distributed process (Koyama et al 2005).
Nocebo Response
Kong et al (2009) found a significant fMRI signal increase to pain in bilateral ACC, left orbital prefrontal cortex (PFC), and right DLPFC. They speculated that changes in PFC and parietal lobule may imply multiple functions, including memory retrieval of previous experience, expectations generation, modulation of pain perception and pain ratings, as well as attention and emotion modulation (J Nueroscience, 28, 49, 13354 to 13362). Repeated negative responses to treatment may reinforce the nocebo response. Therefore it is important to establish in the clients past history their respose(s) to various interventions and to ascertain their expectations of what will and won't help them in future interventions.
Forebrain mechanisms of nociception and pain
"Pain is a unified experience composed of interacting discriminative, affective-motivational and cognitive components, each one of which is mediated and modulated through forebrain mechanisms acting at spinal, brainstem, and cerebral levels. The size of the human forebrain compared to the spinal cord gives anatomical emphasis to forebrain control over nociceptive processing" (Casey 1999, PNAS, 96, 7668 to 7674)
Dissection of perceptual, motor and autonomic components of brain activity evoked by noxious stimulation
Pain, Volume 149, Issue 3, Pages 453 to 462 (June 2010)
M. Pichéacef, M. Arsenaultcde, P. Rainville
Abstract
In the past two decades, functional brain imaging has considerably advanced our knowledge of cerebral pain processing. However, many important links are still missing in our understanding of brain activity in relation to the regulation of pain-related physiological responses. This fMRI study investigates the cerebral correlates of pain (rating), motor responses (RIII-reflex) and autonomic activity (skin conductance response; SCR) evoked by noxious electrical stimulation. Stimulus intensity was adjusted individually based on the RIII threshold to control for differences in peripheral processes and baseline spinal activation. Covariance analyses were used to reveal individual differences in brain activity uniquely associated with individual differences in pain, RIII and SCR. Shock-evoked activity in cingulate, medial orbitofrontal and parahippocampal regions predicted pain sensitivity. Moreover, lateral orbitofrontal and cingulate areas showed strong positive associations with individual differences in motor reactivity but negative associations with autonomic reactivity. Notably, individual differences in OFC activation was almost fully accounted by the combination of individual measures of autonomic and motor reactivity (R2=0.93). Additionally, trial-to-trial fluctuations of RIII-reflex and SCR (within-subjects) were proportional to shock-evoked responses in subgenual cingulate cortex (RIII), anterior insula (SCR) and midcingulate cortex (SCR and RIII). Together, these results confirm that individual differences in perceptual, motor, and autonomic components of pain reflect robust individual differences in brain activity. Furthermore, the brain correlates of trial-to-trial fluctuations in pain responses provide additional evidence for a partial segregation of sub-systems involved more specifically in the ongoing monitoring, and possibly the regulation, of pain-related motor and autonomic responses.
Abbreviations: ACC, anterior cingulate cortex, aINS, anterior insula, AMY, amygdala, BA, Brodmann area, BOLD, blood oxygen level dependant, dlPFC, dorsolateral prefrontal cortex, dPCC, dorsal posterior cingulate cortex, EMG, electromyographic recording, IFG, inferior frontal gyrus, INS, insula, IPL, inferior parietal lobule, MCC, midcingulate cortex, mPFC, medial prefrontal cortex, OFC, orbitofrontal cortex, PAG, periacqueductal gray matter, PCC, posterior cingulate cortex, PCG, precentral gyrus, PCL, paracentral lobule, PFC, prefrontal cortex, pgACC, perigenual anterior cingulate cortex, PHG, parahippocampal gyrus, PMC, premotor cortex, PVA, parietal ventral area, sACC, subgenual anterior cingulate cortex, SCR, skin conductance response, SI, primary somatosensory cortex, SII, second somatosensory cortex, SMA, supplementary motor cortex, VAS, visual analogue scale
Chronic stress and pain
Chronic stress may have a direct influence on pain.
Increased basal mechanical pain sensitivity but decreased perceptual wind-up in a human model of relative hypocortisolism
Pain, Volume 149, Issue 3, Pages 539 to 546 (June 2010)
Linn K. Kuehla, Gilles P. Michaux, Steffen Richtera, Hartmut Schächingera, Fernand Antonb
Abstract
Clinical data have accumulated showing that relative hypocortisolism, which may be regarded as a neuroendocrinological correlate of chronic stress, may be a characteristic of some functional pain syndromes. However, it has not been clarified yet whether deregulations of the hypothalamus–pituitary–adrenal (HPA) axis may directly alter pain perception and thus be causally involved in the pathophysiology of these disorders. To test this hypothesis, we performed a randomized placebo-controlled crossover trial in N=20 healthy drug-free volunteers (median age 24yrs) and analyzed the effects of metyrapone-induced hypocortisolism on quantitatively assessed basal mechanical pain sensitivity (1.5–13m/s impact stimuli), perceptual wind-up (9m/s impact stimuli at 1Hz) and temporal summation of pain elicited by inter-digital web pinching (IWP; 10N pressure stimuli for 2min). Experimentally induced hypocortisolism significantly decreased pain detection thresholds and augmented temporal summation of IWP-induced pain (p<.05). The latter effect was dependent on the relative reduction in cortisol levels, and seemed to rely on a potentiated sensitization and not merely on the observed changes in basal pain sensitivity. Perceptual wind-up by contrast was reduced when cortisol synthesis was blocked (p<.05). This result is reminiscent of findings from animal studies showing a reversal of NMDA receptor activation by glucocorticoid receptor antagonists in neuropathic pain models. Our results speak in favor of a potential causal role of HPA axis alterations in pain chronicity.
Philosophy and pain
An exciting approach to challenging realities is the examination of the Pain and Philosophy of the Mind (Alex Cahana July 2007, Pain Clinical Updates, Vol XV, 5). Cahana argues that 'mind-body supervenience' (physicalism or materilism) where pain always has a physical substrate, isn't enough to explain the qualitative nature/character of pain ("qualia" = what it is to be).
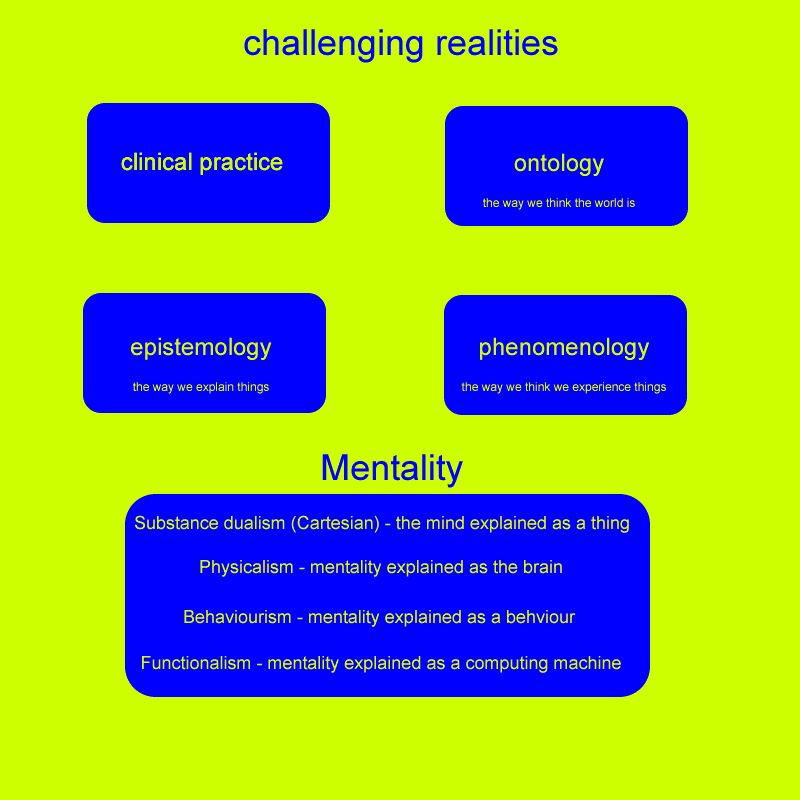
The problem with physicalism as argued by Cahana is that 'you are nothing but your synapses' ("eliminative") or 'you are ultimately your synapses' ("reductive" or "token").

Cahana (2007) concludes by stating that "pain cannot be seperated from the person experiencing it, and the human experience cannot be omitted from a scientific explanation of how our mind works. Therefore, a new subjectivist, interpretive, phenomenological stance is needed in order to capture the complexity of the patient's narrative experience (narrative dyad)".
Thoughts lead to feelings which lead to either action or inaction whereby either activation or deactivation of problem solving takes place. This applies as much to the therapist as to the client who is suffering from pain. Through clinical prediction, environmental prediction can be more finely tuned by the feelings which have preceeded the situation that has taken place. The therapist and the client need to embark in cognitive strategies which include ascertaining feelings and beliefs, appraising the adequacy of the response and then if necessary using problem solving to be able to use realistic goal setting (rather than fear -avoidance behaviour) to establish a paced response. Success (by the therapist and the client) leads to better predictive outcomes and thereby should become self-fulfilling.
Non-dermatomal somatosensory deficit (NDSD) in chronic pain disorders
Egloff et al (2009, Pain, 252 to 258) investigated 30 consecutive patients with unilaterally accentuated chronic pain not explained by persistent tissue damage and ipsilateral somatosensory disturbances including upper and lower extremities and trunk (NDSD). They found that all patients had mild to moderate depressive symptoms (HAMD-17), all had experienced a prolonged antecedent phase of severe emotional distress such as childhood abuse, torture, war, physical or sexual violence, persecution, imprisonment, etc), and most remembered a 'trigger episode of somatic pain' on the affected side. Pain quality was often described as 'burning' associated with 'numbness', a 'sense of swelling' or 'heaviness'. Somatosensory deficits were a replicable hypersensitivity to touch and heat perception of non-dermatomal distribution. Almost 1/3 of patients had hyposensitvity extending to the facial area including hyposensitivity, slightly hanging mouth corner or pseudo-ptosis. Parodoxically, the hyposensitvity to touch was combined with increased sensitivity to deep muscle palpation (similar to fibromyalgia) and joint palpation in the painful area. Imaging with FDG-PET showed a significant hypometabolic pattern of changes in cortical (primary somatosensory cortex) and subcortical areas, mainly in the post-central gyrus, posterior insula (regarded as a secondary centre of temperature and vibro-tactile discrimination in space and also of pain perception), putamen, and ACC. Prevelance of NDSD ranges from 25% to 45% in chronic pain complaints (Gagnon & Nicholson 2009, Pain, 12 to 13)
Motor control in the presence of pain
A 'Pain-Adaptation' model was coined by Lund et al (1991) which hypothesised that movement velocity and amplitude is reduced in the presence of pain with reduced agonist activity and increased antagonist activity in limb and jaw movements. In the trunk this may mean increased coactivation of the superficial muscles at the expense of the deeper postural muscles. This is significant as Bergmark (1989) differentiated muscles based on their segmental stabilising role versus their global mobilising role. The pain-adaptation hypothesis suggests that the global mobilisers inappropriately become the stabilisers of the spine, which can lead to excessive splinting and compress spinal structures.
Pain Processing
Clearly, chronic pain may change the structure of the brain. Traditionally, pain impulses were though to affect cortical activity in a fixed manner. However, it can be seen by the previous discussion that cortical interaction not only is influenced by pain impulses (bottom - up) it can also change the interpretation of pain impulses, as well as change the behaviour towards those impulses (top - down). The brain is remarkarbly malleable to change, demonstrating functional (and dysfunctional) plasticity to various management strategies.
The brain exhibits plasticity and therefore is malleable to change.
The role of values in a contextual cognitive behavioural approach to chronic pain
The experience of chronic pain can be an overwhelming one. Pain and other unwanted experiences can become the focus of daily efforts while less time is devoted to family, intimate relations, friends, work, health, or developing as a person. This can be viewed as a failure of their efforts to serve important interests, or a failure of their 'values' to guide their actions (McCracken & Yang 2006, 123, 137 to 145). Acceptance of pain can be viewed as a weakening of pain to guide their actions whereas 'value-related' processes, involve a strengthening of guides for action that are unrelated to pain, but rather actions guided by the individual to live their life according to what they care about most deeply. McCracken & Yang (2006) examined patient values in the domains of family, intimate relations, friends, work, health, and growth or learning. They found that highest importance was placed on the values in the domains of family and health and the least importance in friends and growth or learning. Highest success was reported in domains of family and friends and the least success in health and growth or learning.
Values are essentially verbally constructed desired life directions. Values clarification can be seen as the adding of cognitive influences to patterns of behaviour. Values based methods can bring into therapy a focus on whether the patient is taking action in their life that serves what they care most about (McCracken & Yang 2006)
Contextually based clinical approaches to human suffering and behaviour problems address cognitive processes differently than is typically done within a traditional cognitive-behavioural approach (McCracken 2005). Rather than attempting to alter the form or frequency of maladaptive thoughts, contextually based approaches aim to alter their function, how they are experienced, or how they influence other behaviour. Therapeutic effort approaches concerns loosening unadaptive cognitive influences on behaviour and increasing behavioural flexibility by processes such as 'mindfulness' and what is referred to as cognitive de-fusion. Mindfulness has been significantly related to multiple measures of patient functioning (McCracken et al 2007, Pain, 131, 63 to 69).
Mindfulness can be defined as the practice of broad, present-focused, and behaviourally neutral awareness. It is a way to observe experiences, such as physical symptoms, emotions, or thoughts, such that some of the otherwise automatic behavioural influences attached to these experiences are reduced, leading to more balance, non-reactive, and realistic contact with situations, and more effective action (McCracken et al 2007).
The goal of mindfulness is not to alter the content of what is experienced but to change how it is experienced and the influences it exerts on behaviour. Mindfulness is best understood in a functional and contextual framework rather than challenging or modifying thoughts and feelings. In the chronic pain scenario, changing what is felt is far more difficult than changing the behaviour in relation to what is felt which suggests that mindfulness could play an important role in multifactorial treatment approaches. MIndfulness includes noticing and not reacting to pain, emotions, urges, thoughts, and other feelings in the body thus freeing the person for function and movement. "Full present focus and non-reactive awareness" (McCracken et al 2007) would be a goal of a multifaceted management strategy.
Assessment - Factor Web
Methods for assessing the influence of extraneous pyscho-social varaibles are many fold and generally reflect the multi-dimensional nature of pain and suffering. The NZACC has developed a clincal assessment guideline to aid in the management strategy. The results of this assessment are used to predict final outcomes. Hereby, the form of the optimal management strategy can be implemented at an early stage which should either lead to faster recovery or at least reduce the likelihood of the secondary affects of chronicity. These clinical decisions on whether to be hands-on, hands-off, or to use CBT focused on content versus a focus on education can be used by the clinician to rationalise expected treatment outcomes. This latter aspect of education is consistent with the concept of the malleable brain, where the recognition of the affect of reverberating dysfunctional neuronal generators can be used to help the client 'move-on' , and help themselves get out of the rutt which their sufferring has brought them.
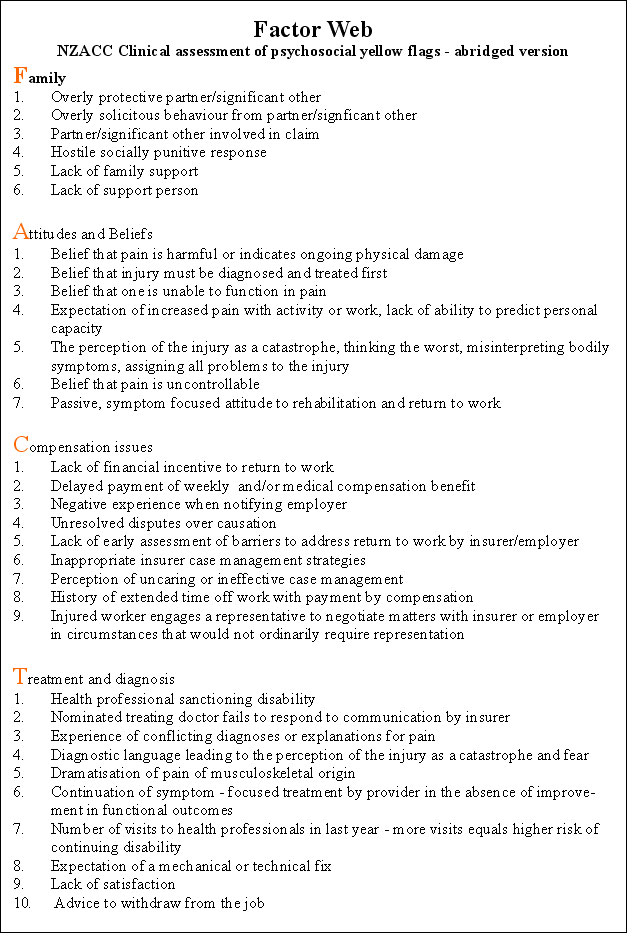
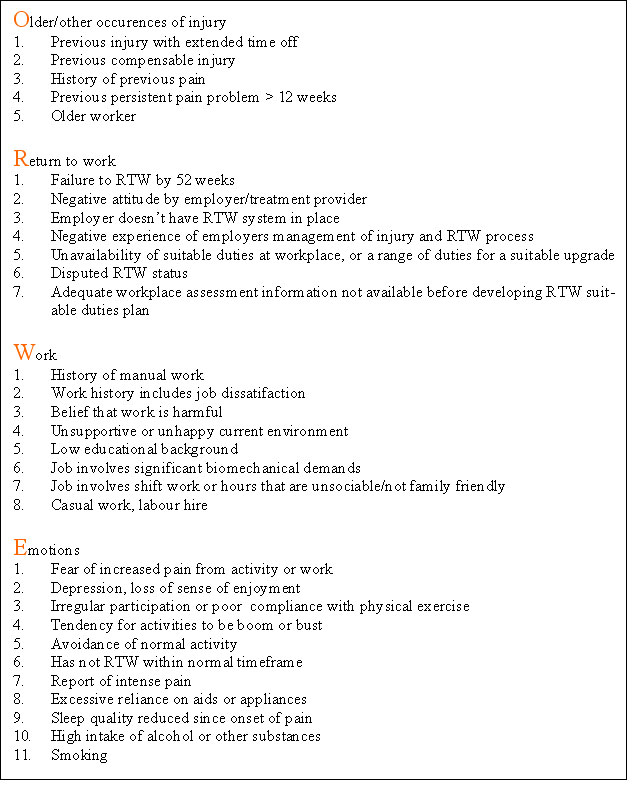
Hewitt, Hush, Martin, Herbert & Latimer (2007), AJP, 53, 269 to 276, established that measures of activity limitation and pain at 9 weeks, and work status at 6 months have the greatest predictive accuracy of someone developing chronic pain and disability.
Assessment - Psychometric evaluation
It is easy to be overwhelmed by such multiple factors which could contribute to chronic LBP. However, we must evaluate what is relevant and use this differentiation to determine what our strengths and weaknesses are as a profession and when to refer to other professionals. Importantly, there will be a significant subgroup of clients who have chronic musculoskeletal injuries due to mismanagement, which if identified could be resolved through multi-factorial physiotherapy which includes passive techniques, exercises and education.
The ICF - WHO has stipulated three seperate but related dimensions of functioning are defined as body dimension (functions and structure), individual dimension (activity), and social dimension (participation). Body functions are physiological or psychological functions of body systems. Activity describes daily purposeful integrated body systems execution of tasks. Whereas participation deals with the experiential and contextual setting of the persons life (social relationships, employment, and economic life), as well as societies response to the person's level of functioning.
According to Thonnard & Penta (2007), Eur Medicophys, 43, 525 to 541, "rehabilitation can be defined as a reiterative problem solving and educational process that focuses on disability (altered activities) and aims to maximise participation in society while minimising the stress on and distress of the patient and family". While the outcome of a particular physiotherapeutic intervention can be stipulated based on functional measures, these need to be validated not only w.r.t diagnosis but also their meaning w.r.t the participation of the patient in the community. The latter hasn't specifically been addressed and has frequently been assumed to correlate with functional status. Importantly, functioning and participation in the community are highly likely to be key measures when it comes to financing treatment interventions.

http://www.sf-36.org/tools/SF36.shtml
Modified Schober Test (MMST) tests range of movement in the lumbar spine in the ICF dimension of body function. Validity as correlated to X-ray is 0.67, reliability as an inter-rater score is excellent (ICC=0.95, 95%CI, 0.44-0.84), responsiveness (sensitivity) requires a change of over 1cm to be 95% confident of change.
Thonnard & Penta (2007), Eur Medicophys, 43, 525-541
Low Back SF-36 tests both ICF dimensions of body functions and activities. 18 items pooled from the Australian low back SF-36, modified version of Oswestry and Quebec back pain disability scale has fewer misfitting items than the original SF-36 and thus elimates it's floor and ceiling effects. Unidimensional linear scale developed with the Rasch partial credit model. Inter-rate reliability were 0.94. The minimal detectable change is 12 points on a 100 point scale.
Thonnard & Penta (2007), Eur Medicophys, 43, 525-541
Physical Impairment Index (PII) evaluates physical impairment in LBP through 7 tests, each scored dichotomously based on published cut-offs. ICF dimension of body function and structure. Convergent validity was supported by correlations with disability (r=51 w.r.t. Roland Morris Q'naire), work loss in past year (r=0.43), pain (r=0.27), depression (r=0.26 with Zhung depression inventory), somatisation (r=0.32 with modified somatic perception Q'naire), non-organic signs (r=0.49) and non-organic symptoms (r=0.35). Correlations were also found with the physical component of the SF-36 (r=0.28) and physical activity subscale of the fear-avoidance beliefs questionnaire (r=0.24). Good to excellent reliability for individual items (ICC from 0.48-0.96). The overall score demonstrated excellent inter-rater reliability (ICC=0.89)
Thonnard & Penta (2007), Eur Medicophys, 43, 525-541
Roland Morris Questionnaire (RMQ) self administered disability measures in LBP reflecting 24 activities of daily living. ICF dimension of activities. The responsiveness is sufficient to detect change after 4 to 6 weeks of physiotherapy in patients with an initial score in the central portion. However, the magnitude of error is too large to detect improvements in patients with a score of less than 4 and deterioration in patients with scores of greater than 20.
Thonnard & Penta (2007), Eur Medicophys, 43, 525-541
Sickness Impact profile (SIP) is a behaviourally based measure of perceived health status applicable across a spectrum of illnesses and among various demographic and cultural subgroups, applied in LBP with an ICF participation dimension. Validity has been reported with various biological and clinical measures and subcategories of the Minnesota Multiphasic Personality Inventory. High test-retest reliability coefficient (r=0.85) in LBP.
Thonnard & Penta (2007), Eur Medicophys, 43, 525-541
Chronic Pain : Global Physiotherapy Examination 52 (GPE-52) is a clinical physical examination in 5 domains including posture, respiration, movement, muscle and skin palpation. Good to excellent inter-rater reliability of the total score (ICC=0.91), and individual components (ICC=0.65 for posture, 0.60 for respiration, 0.89 for movement, 0.83 for muscle palpation, 0.76 for skin palpation). However, requires 3 days of training and some 30 minutes to complete.
Thonnard & Penta (2007), Eur Medicophys, 43, 525-541
Orebro Musculoskeletal Pain Questionnaire (OMPQ) is a "yellow flag" screening tool that predicts long-term disability and failure to RTW when completed over 4 to 12 weeks following soft tissue injury. A cut off score of 105 has been found to predict those who will recover (95% accuracy), those who will have further sick leave in the next 6 months (81% accuracy), and those who will have long term sick leave (67% accuracy). In workers with back injuries, at 4 to 12 weeks, a cut-off score of 130 correctly predicted 86% of those who failed to RTW.
The Impact of Event Scale (IES) was developed to measure current subjective distress related to a specific life event (Horowitz M et al 1979, Psychosom Med 41, 209 to 218).Two response states, avoidance and intrusion are measured. The IES has 15 items, seven of which are intrusive symptoms such as thoughts, nightmares, feelings, and ima ges associated with a specific event. Five of these measure intrusive symptoms whilst awake, whereas 2 others measure intrusions at night (insomnia, nightmares). The avoidance subscale has eight items such as a numbing of responsiveness, and avoidance of feelings and situations. A cut-off of 26 or above would be grounds for a psychological referral. However, a few weeks may be allowed to pass as to allow some natural recovery. Has been recommended by Dr Michelle Sterling in some people who have suffered a whiplash type injury.
The Pain Self Efficacy Questionnaire (PSEQ) ask clients to rate how confidently they can perform the activities despite their pain. It covers a range of functions including household chores, socialising, work as well as coping with pain without medication. It is based on Bandura's (1977) conceptualisation of self-efficacy as a reflection of a resilient self-belief system' in the face of obstacles. Takes 2 minutes to complete. Low scores 40 suggest that the client is likely to respond well to an exercise regime. Low PSEQ is a predictor of long term disability and depression.
The Pain Anxiety Symptoms Scale (PASS) validity has been supported by positive correlations with measures of anxiety, cognitive errors, depression, and disbaility.
Fear of Work Related Activity = Fear - Avoidance Beliefs Questionnaire (FABQ) has 2 parts, one on physical activity, the other on work. The latter has been shown to have significant predictive validity with disability in ADL and days off work, more so than biomedical parameters such as anatomical pattern of pain, temporal pattern, and pain intensity.
Fear of movement = Tampa scale for kinesiophobia (TSK) is a 17 item scale to assess the fear of re-injury due to movement.
Identification of personal and environmental factors provides the opportunity to incorporate these elements into treatment strategies with appropriate interventions such activities based on cognitive behavioural strategies.
Assessment Physical


The brain can filter as well as amplify incoming information (see musculoskeletal neurophysiology section ). Cognitive behavioural therapy uses goal setting and feedback to favourably access the central nervous system towards goal specific movement
Management & Treatment : Reducing Pain-Related Fear
Peter Lang's bioinformational theory of fear (J Affective Disorders 2000; 61:137 to 159) predicts to reduce fear
- the network mediating the fear needs to be activated
- new information needs to be presented to discredit the expectations that are inherent to the fear memory.
Demystification of the pain through education, appropriate treatment with graded exposure which includes operant cognitive behavioural activity parameters are the cornerstone of such an approach. Paradoxically, verbal re-assurance may have the opposite affect and lead to increased distress. When pateints experience the reassuring information as a lack of understanding of the legitimacy of the complaint, they were found to respond by asserting the complaints more forcefully (Salmon 2006, CNS Spectrum, 11, 190 to 200). Reassurance " removes the fears or doubts of pain/illness" and takes place in the dynamic intereaction between caregiver whose intent is to reduce worry, and the patient who is concerned. The psychologycal literature suggests that direct attempts to change thought or beliefs, such as providing information, are not as effective as experienced-based methods (de Jong et al 2005, Pain, 21, 9 to 17). Furhtermore, the use of diagnostic results seem to only reduce 'worry' in the short-term and hence provide no clinical value and even worse have been reported to decrease patient reported well-being (Linton , McCracken, Vlaeyen 2008, Pain, 134, 5 to8). Expressing empathy may be a critical element in reassurance, which comprises the acknowledging and understanding of what the patient is experiencing and includes elements of respect and understanding (Goubert et al 2005, Behav Res Ther, 43, 1055 to 67). These people frequent desire more emotional support rather than more explanations or information. Empathy may allow the patient to engage in treatment rather than focus on having their symptoms understood or believed (Jensen 2002, In Turk &Gatchel, Psychological approaches to pain management: a practitioner's handbook, The Guilford Press, p71 to 93)
Treatment - reduction in catastrophising
Poorer disability outcomes are promoted by unhelpful and overly alarmist beliefs (catastrophising) about pain and injury, which in turn lead to increased fear of movement and hypervigilance for pain, resulting in avoidance of activities expected to aggravate pain, an ultimately prolonged disability, depressed mood and more troubling pain (Nicholas 2009 Pain, 145, 6 to 7). Importantly, it may not be the baseline factors which predict a return to work, but rather the sequential reduction in catastrophising, fear of movement and severity of pain which best predicts functional outcome (Nicholas 2009). However, in acute LBP, fear of movement appears to be more predictive of functional disability than pain intensity or catastrophising (Swinkels et al 2006).
Evidence to support this come from
- Swinkels et al (2006, Pain, 120, 36 to 43) where in n=96 people with acute LBP, they found that pain-related fear, as measured on the Tampa Scale for Kinesiophobia, was the strongest predictor in a physical lifting task. Using the Roland-Morris Disability Questionnaire as a measure of percieved disability, both pain-related fear and pain catastrophising, as measured with the Pain catastrophising Scale, were significantly predictive of perceived disability and more strongly so than pain intensity was.
- Patients in 'graded in vivo exposure' (GivE) conditions demonstrated significantly greater improvements on measures of fear of pain/movement, fear avoidance beliefs, pain-related anxiety, and pain self-efficacy when compared to a graded activity programme and significantly greater improvements on measures of fear-avoidance beliefs, fear of pain/movement, pain related anxiety, pain catastrophising, pain experience, and anxiety and depression when compared to people on a wait list. (Woods & Asmundson 2008, 136, 271 to 280)
- GivE involved educating the patient about the cognitive behavioural perspective on fear-avoidance and its consequences, followed by the application of graded exposure techniques
- Formulation of the patients problem within context was accomplished by establishing an indiviualised hierarchy of fear-elicitng movements using the Photograph Series of Daily Activities (PHODA; Kugler et al 1999 Institute for Rehabilitation Research and School of Physiotherapy, Heerlen, The Netherlands).
- Boersma et al (2004, Pain, 108, 8 to 16) used PHODA which included 98 photographs that represent ADL such as lifting, bending, bicycling, vacuum cleaning, making the beds, etc. Personal goals and goals established by PHODA were used to establish a heirarchy of ordinary movements and activities. n=6. Period of GivE was between 3 - 4 weeks and the trial went for 10 weeks. The results demonstrated decreases in rated fear and avoidance beliefs while function increased substantially.
Improved ability to predict pain, results in a decrease in hypervigilance and threat evaluation which in turn results in a decrease in anxiety and avoidance, and reductions in catastrophising (Woods & Asmundson 2008)
Neurolinguistic programming and Cognitive Behavioural Therapy should be incorporated into the overall management approach
Neurones which fire together function together. Abnormal, excessive neuronal firing to 'perceived threats' can be extinguished through behavioural responses associated with positive physical activity, substitution through imagery as well as teaching appropriate self -appraisal techniques. Graded exposure to stressful situations can aid in re-establishing correct allostasis.
Chronic pain may be the lack of recognition of 'safety signals' and/or hypervigilance of perceived 'danger signals'

Examples of the interaction between thinking, behavior, emotion and physical feelings
| Cognitive | Behavioural | Emotional | Physical | ||||
| Start | End | Start | End | Start | End | Start | End |
| Never going to get better | I have leanrt from other peoples problems | Avoiding activity | returned to sport | irritable | I feel calmer | constant high pain levels | I am much less aware of pain |
| Fearful of damage | Learnt problem solving skills | Disabled, slouching, head down | gym three times per week | Grumpy | It's hard for everyone | Holding body | I am more relaxed |
| I feel like a failure | I understand the system and the insurer doesn't bother me | Seeking weekly treatment | ceased treatment | socially inept | confident | pain provoked with minor activity | I feel stronger |
| Bleak future | pain does not equal damage | withdrawn socially | socially interactive | depressed | happy | painful thickened soft tissues | my muscles feel incontrol |
| Unable to play sport or work | I don't worry about pain now | unable to help self | doing enjoyable activities | helpless | relaxed | decreased resilience | my body feels energised |
| Confused about future | thinking positively | victim | I have a steady relationship and I have moved out of home | Frustrated | Enjoying life | spasms of lumber extensors | I can move and exercise without flare-up |
| Bulging disc is causing my pain | Bulging discs are normal and become pain free | Holding breath | doing breathing/relaxation techniques | Angry | It's not worth worrying about | deconditioining | I am getting fitter |
| I am avoiding bending | Bending with safe lifting technique | Tense | I feel more relaxed |
from Peter Roberts, Paragon Institute Pain Management Program, Adelaide. In SportsPhysio, 2007, 4,15 to 17
Socratic Questioning - the use of provocative questioning to overcome peoples underlying assumptions and beliefs
- What are the facts and what are my subjective perceptions?
- What is the evidence which supports my perceptions?
- What is the evidence which contradicts my perceptions?
- Are there thinking errors?
- How else can the situation be perceived?
Behavioural Disputing - while behaviours can reinforce unhelpful cognitions, they can be used to dispute them. Behaving in a way that is inconsistent with certain cognitions can help us discover that those cognitions are incorrect.
Goal Directed Thinking - involves focussing on the self-defeating nature of our cognitions, recognising that our current perceptions prevent us from achieving the things we want. In goal-directed thinking we remind ourselves to remain focused on our goals.
Overcoming Low Frustration Tolerance (LTF) - overcoming the use of 'shoulds', 'black & white' thinking, catastrophising, use of extremes "always" can occur by using the
Antecedents Beliefs Consequences & Disputes
A B C D
Examine
-
the situation which triggers the response
-
the cognitions about the situation
-
the way that we feel and behave
-
disputing the belief
CBT employs cognitive and meta-cognitive process by examining the
-
situation
-
feelings
-
thoughts
-
beliefs
-
thinking errors
Instituting a
-
disputing strategy
through
-
positive actions
This methodology can be used to improve mental, emotional and physical well-being.
Several lines of evidence suggest that treatment using the psycho-cognitive domain to evaluate perception can substantially influence treatment outcome. It would appear that fear-avoidance and distress are important factors in the development of pain-related disability (Boersma & Linton 2005). Clients with higher treatment expectancy demonstrated better pain coping and control, active and positive interpretation of pain, and less disability compensation. Additionally, these positive perception attributes significantly predicted post CBT outcome measures in people suffering chronic pain (Goossens et al 2005). Perception has been demonstrated to be positively influenced by educational sessions where fear reductions significantly decreased pain intensity through graded exposure and this remained up to 6 months post intervention (de Jong et al 2005). Psychometric evaluation strategies such as the Chronic Pain Coping Inventory (CPCI) provides clinicians with a measure of the frequency with which patients use coping strategies, which are both encouraged (exercise/stretching, relaxation, task persistence) and discouraged (guarding, resting, asking for assistance) (Jensen et al 1995). Therefore, adherence to positive coping strategies may be evaluated and correlated with any changes to perception traits such as reduction in 'fear-avoidance' behaviour
Treatment techniques for central programming errors of somatosensory, occular and vestibular information
-
Adaptation
Resetting or retuning movement systems and perception thresholds through adaptation via repetitive and provocative movements. This requires voluntary motor control and mental effort. Requires 1-2minutes of practice with error signal and must be context specific. Exercise needs to achieved at the limit of ability and not the limit of comfort. Perception needs to be challenged
-
Substitution
Physiological or behavioural mechanisms are used for re-learning(substitute) sensory strategies during functional tasks. Examples include teaching the person to attend to various inputs by switching to various body regions using interoceptive feedback and switching to external sensory systems for extroceptive feedback (smell, eyes - vision & balance, and ears - sound & balance). Additionally, some inputs can be removed or altered such as foam under the feet whilst standing. Behavioural coping strategies, education and relaxation techniques can be used here to learn how to lessen the experience of the symptoms. Visualisation of successful execution of provocative tasks using an internal frame of reference whereby the painful experience is not the dominant experience can also be used.
-
Habituation
Habituation uses repeated exposure ot noxious stimuli to bring about neural changes to reduce sensitivity to the stimuli. Importantly, the source of competing sensory information needs to identified. Movements need to be designed based on those reproducing symptoms (1-4movements, 2-3 x per day, 2-5 x per week). May take 4 weeks to notice change. Should be carried out for at least 2months.
Happiness
Happy people tend to have personal attributes linked to good self esteem, a sense of control, optimism and extroversion. Extraneous factors associated with happiness include work, consuming interests (having a passion for something), having goals (a sense of mission or purpose in life), relationships (intimate vs superficial, happily married, happily single), religion, and active lifestyles.
When dealing with someone with chronic pain/disability, it is worthwhile ascertaining
- how satisfied they are with their current lifestyles
- whether their lifestyle reflect their beliefs of what is important (eg believe exercise is important but do not have time to exercise)
- if their current lifestyles will bring about the things they wish for in the future
Factors associated with happiness which will affect the overall prognosis are
- work/regular commitments
- interests/leisure activity
- mental stimulation
- health maintenance
- relationships
Dr Sarah Edelmann (2006) quotes Dan Milliman (No Ordinary Moments)
"Knowing what to do is not usually the problem. The elusive goal is translating intentions into action and resolutions into results. The gap between knowing and doing remains a weak link in most of our lives" (Change Your Thinking, 2nd ed, ABC books Sydney, p273).
In terms of physiotherapy we must examine beliefs and intentions. By assessing these constructs at the initial subjective examination, the physical examination can be planned. Furthermore, through this interaction between therapist and client, prognostic goals can be prescribed which are realistic, relevant and purposeful to all people involved in the management process. Hereby, intentions are translated into actions and resolutions become results. In this manner expectations can be managed and energy can be focused/chanelled into the right direction.
Non specific low back pain
When the 5th international congress in low back pain concluded in Melbourne (Nov 2004), apart from the usual palabra, there seemed to be some common sense coming from the floor into the discussions. The great proponents of reductionist paradigms for studying so called 'non-specific low back pain' came under fire for the 10 years of misdirected and misguided research trying to identify specific variables using a non-specific paradigm. Cognitive factors, including beliefs, depression, kinesiophobia were thought to make up around 50% of measurable outcome variables, disability 30% and impairment only 20%. Whilst the statistical methodology & reasoning was highly commendable, the premise of a lot of research on the efficacy of treatment interventions was that all physiotherapists are equal. It would seem ludicrous that the same proponents of graduate programmes in Musculoskeletal and Sports Physiotherapy can rationalise that the skill level of the physiotherapist is irrelevant to outcome. These arguments seem to have arisen from poorly designed investigations in the mid 90's.
Impairment measures are traditionally seen as 'range of movement' and sometimes neurological impairment. However, more difficult measures which usually aren't included in impairment measures are quality of movement, and the muscle activation required for the distribution of force across joints and between body segments (inverse dynamics and Newtons 3rd Law). Additionally, when considering the 'mass-spring' analogy of movement and energy conservation, then perturbations of movement and the capture of energy from perturbations of movement, such as plyometrics , become important aspects in the clinical reasoning paradigm. Yet, how are these measured in the NSLBP paradigm by traditional 'non-progressive' research.
Those same protagonists also argued in the 1990's that there was no role for dose in manual therapy. (Dose representing the force, duration, frequency, number of repetitions, the type of technique used commiserate with the stage, stability, severity and irritability of the disorder as well as based on the identification of the 'cause of the cause' of the dysfunction). Additionally, back in the 1990's they used placebo constructs which ignored the fundamental role of higher centres in pain and information processing. Even the paper which I submitted to Manual Therapy for publication in the mid 90's on mechanical traction had the descending modulation and cortical modulation aspects deleted from it by the co-authors.
Thankfully, since the mid 2000's multi-modal treatment approaches are receiving credibility as a research paradigm. Additionally, the biomechanics and specific treatment intervention for pelvic girdle dysfunction is being extracted out of the NSLBP paradigm. Progressive research on impairment and specifically the importance of muscular forces are being performed by Wim Dankearts under the guidance of Peter O'Sullivan. They are working towards a novel classification system for non specific chronic low back pain patients which includes higher order mental processing. Simply stated patient classifiction have taken both a behavioural and direction specific functional approach. Specifically, Peter O'Sullivan has put forward 3 sub-categories
-
"Pain disorders associated with movement impairments are associated with a loss of normal physiological movement of lumbo-pelvic mobility, and abnormally high levels of muscle guarding and co-contraction of lumbo-pelvic muscles with generation of intra-abdominal pressure....[resulting in].....excessive force closure"
-
"Pain disorders associated with control impairment are associated with no impairment to the mobility of the symptomatic spinal segment, but rather present with impairments or deficits in control of the symptomatic spinal segment pressure...[resulting in]....reduced force closure"
-
"......mal-adaptive movement and motor patterns result in chronic abnormal tissue loading and ongoing pain and distress......These disorders are also invariably associated with non-organic factors but these factors do not dominate the disorder, leaving them more amenable to physiotherapy intervention based on a cognitive behavioural motor learning model"
(5th Interdisciplinary World Congress on Low Back and Pelvic Pain, Melbourne, 2004, Australia p132)
O'Sullivan (2005, 2007 Manual Therapy, 11, 169 to 170) described 3 main classification groups in people presenting with chronic disabling back pain
- the first group appears to be presented by subjects where movement impairent and motor dysfunction is secondary and adaptive to underlying pathology such as inflammatory pain, neurogenic pain, neuropathic or centraly mediated pain disorders, severe structural disorders
- a second group exists where a dominance of psychological and/or social (non-organic) factors are underlying the drive of the disorder. This results in latered pain processing, amplification of pain and resultant disorderd movement and motor dysfunction. In these two groups, attempts to simply normalise the motor dysfunction and movement impariment are likely to fail
- a third group exists where maladaptive and dysfunctional movement patterns result in abnormal tissue loading and ongoing pain and distress. These people can present in two manners
'movement impairment' characterised by avoidant pain behaviour and a loss of lumbopelvic mobility in the direction of pain. These movements are usually accompanied by an inordinately high level of muscle guarding and cocontraction of lumbopelvic muscles. This is usually accompanied by fear of movement into the painful pattern, as well as faulty coping strategies and beliefs regarding the pain disorder
'control impairment' with no impairment to the mobility of the symptomatic spinal segment in the direction of pain provocation but rather the impairment involves the motor control aound the neutral zone of the motion segment or the segment finds itself fixed at the end of range in the direction of pain. Patients adopt postures and movement patterns which are maladaptive & provocative (not avoidant)
Flexion dysfunction
- impairment into flexion, maintaining high lumbar/low thoracic lordosis whilst the low lumber spine remains in kyphosis, pelvic posture tends to be posterior in sitting, long sitting, sit to stand and squatting, repositioning tends to overshoot into flexion, reduction in extension at the symptomatic level, use of hands to return to neutral, arc of pain, in 4 point kneeling and sitting they show an inability to initiate movement with a neutral lumbar spine at the low lumber levels
Lateral Shift dysfunction
- usually assoicated with a forward bending and rotation injury
- display a characteristic shift of thorax on pelvis, reduced/absent multifidus activity on the contralateral side of shift, increased iliopsoas, erector spinae and quadratus lumborum acitivity on the side of shift, lateral flexion is accompanied by translation rather than rotation of the vertebrae, attempts at neutral result in cocontraction of the diaphragm and quadratus lumborum and sometimes the multifidus on the side of shift, shift is accentuated when standing on the foot ipsilateral to the side of thoracic shift, arc of pain and deviation, report relief when standing in lordotic posture
Active Extension pattern
- tendency to maintain increased erector spinae activity thereby increasing the force closure, repositioning tends to over-shoot into extension, thorax anterior to pelvis, anterior pelvic tilt, use of hands to return from forward bending, inability to slouch, inabaility to posterior pelvic tilt without the excessive use of rectus abdominis, external obliques and hip flexors, inability to co-contract the lumbar multifidus and transverse abdominis with a tendency to hyperextend and overactivate segmental extensors and inability to control diaphragmatic breathing, hip extension with knee flexion results in hyperlordosis with loss of abdominal cocontraction with inner range erector spinae and hip flexor overactivity, pain into flexion due to the inability to reverse the lumbar lordosis
- mechanism of injury is usually in extension, occassionally in foward bending where the lumbar spine was held in extension. Aggravating movements include foward flexion, activities which include extension such as foward sitting, overhead reaching, fast walking, swimming, and running.
Passive Extension pattern
- tendency to passively lever into extension, thorax tends to be posterior to pelvis, generalised reduced muscle tone in erector spinae, multifidus, transverse abdominis with increased tone in the rectus abdominis and external obliques, in sitting a tendency to slouch, re-positioning tendency to over-shoot into extension, inability to posterior pelvic tilt without excessive activation of the upper abdominal wall and thoracic flexion, no pain into flexion as they are able to reverse their lordosis, flexion relieves symptoms
- mechanism of injury associated with extension
Multidirectional
- mechanism of injury is usually traumatic, highly debilitating with excessive hinging and shifting in all movement directions
The classification system of Peter O'Sullivan would suggest that once the condition has progressed to a stage of neurogenic inflammation and neuropathic pain then intervention by Musculoskeletal Physiotherapy will be of little value and referral to a pain clinic would be more appropriate.
Motor Control and Functional Stability
The Bernstein perspective of functional stability suggests that the body regulates it's movement by using a stable reference of control. This reference of control may be the summation of the muscle tension and neural input around the joint (see shoulder for an example). Additional input comes from the visual and vestibular systems. Normally, the central nervous system uses feed-forward mechanisms of control whereby descending electrical input on the spinal cord neurones interacts with afferent input from the periphery. This afferent input comes from the maintenance of tension in the nuclear bag and nuclear chain fibres thereby generating concomitant firing of annulospiral endings which provides a loop between alpha-gamma efferent control and type Ia and type II afferent feedback. Moreover, the movement controller appears to be capturing the momentum of oscillating body segments.
In the presence of pressure on nerve fibres, inflammation and/or pain the afferent input changes resulting in muscle spasms, weakness, loss of co-ordination and reduced proprioception (see Neurophysiology section for more details). Immune system compromise will also alter the functioning of the muscle from an organ of movement to an organ that provides proteins for immune function and organ health. Additionally, efferent firing from the peripheral sympathetic nervous system can change muscle tone as well as blood flow. Finally, cognitive factors such as emotion and fear-avoidance behaviour will influence peripheral muscle tension. Taken together, the functional stability of the system may be compromised leading to either excessive stiffness (force closure) or excessive movement. Either scenario will lead to inefficient use of energy creating unwanted movements in other parts of the body. The laws of inverse dynamics dictate that accelerating body parts will have equal but opposite reactive forces placed upon them resulting in the transfer of energy across the kinetic chain (e.g. foot-knee-hip-back). Therefore, pain and inflammation creates suboptimal biomechanics which can lead to further inflammation and pain in additional areas where these unwanted forces have been directed. For example tight hamstrings &/or early hamstring contraction concomitant with late relaxation of rectus femoris &/or tight rectus femoris can result in counter-nutation and shear across the sacroiliac joint and lumbar spine. This is important as form closure and force closure biomechanics suggest that the pelvis is only stable when the sacrum is nutated. Additionally, tightness of the piriformis creating contralateral SIJ pain due to torsion of the sacrum can also occur. In the former case the client will present with difficulty moving in the saggital plane. In the latter case the client will have problems with unilateral weight bearing. These scenarios can lead to severe intractable pelvic girdle pain, which will require muscle energy techniques and appropriate functional exercises to treat.
Stages of motor learning according to Peter O'Sullivan
- First stage of learning - cognitive stage :
- develop an understanding of the way their movement influences their pain. The use of biofeedback such as touch, vision, video, mirrors, etc is critical at this stage. The first aim is to introduce a neutral lordosis without the use of hips and upper lumbar spine - thorax. Patients with a flexion pattern or lateral shift may need to commence with facilitation of anterior pelvic tilting and low lumbar spine lordosis independently. Best taught in supine crook lying, 4 point kneeling and sitting. However, the correct position of thorax on the pelvis must be attained when training in sitting.
- In active extension pattern the reverse will be required with a need to flex the lumber spine. This is best done in crook lying to facilitate the spine into posterior pelvic tilt
- For passive extension pattern the focus is to achieve neutral lumbar spine at the level above the unstable segment, whilst maintaining the pelvis and unstable segment in neutral. The upper abdominals need to be deactivated and this is best achieved in sitting with the thorax anterior to the pelvis to minimise the affect of gravity on the upper abdominal wall.
- Once lumbar neutral is achieved emphasis for : flexion patterns is activation of lumbar mutlifidus and psoas with co-activation of the pelvic floor and transverse abdomninal wall muscles without co-activation of erector spinae; lateral shift patterns is acitvation of the unilateral multifidus and psoas; for active extension the focus is on pelvic floor and transverse abdominal wall without activation of the erector spinae; for the passive extension group the emphasis is on coactivation of the transverse abdominal muscles, psoas, and multifidus whilst inhibiting the upper abdominal muscle
- Second stage of learning - associative stage
- fine tuning incorporating the maintenance of lumbar lordosis with dynamic tasks or static postures. Previously painful movement tasks are broken down and the co-contractions are performed in the component parts. For example sit -> stand is commenced in sitting, then leaning foward, weight transference through the hips, then taking weight onto the feet. For flexion patterns there will be a tendency to loose anterior pelvic tilt and low lumbar lordosis with an accentuation of the lordosis higher up, in the lateral shift group there will be a similar tendency but also with a shift of weight to one side, whereas in the active extension group there will be a tendency to posterior pelvic tilt and increase lordosis during load transfer as well as loose the transverse abdominis
- the aim is to identify 2-3 faulty movement patterns and break them down into their component parts and do 40-50 repetitions. Be aware of the breakdown of movements due to fatigue. They should practice at home, gradually increasing the speed and complexity of the movements. Additionally some form of aerobic exercise such as 30minutes walking has been recommended. This stage can last from weeks to months.
- Third stage - automated stage requires little attention with higher loading cardiovascular conditioning (O'Sullivan et al 1997 In Grieves Modern Manual Therapy, 2005, Elsevier, 325 to 328)
Further leg muscle-pelvic considerations
The gluteal muscles of the stance leg requires counter-stability by the contralateral latissimus dorsi and erector spinae (Newtons 3rd law). The attachment of the latissimus dorsi to the transverse abdominis may lead to additional stability. The rotation of the pelvis, being controlled by the stance hip rotators (iliacus, piriformis, obturators) and gluteus medius are countered by the internal oblique and opposite adductor longus. Hereby, rhythmic oscillation of body parts capturing and releasing momentum leads to efficient motion.
The inferior gluteus maximus is used during running and fast walking to bring the foot down onto the ground just prior to stance. Clinically, the inferior gluteus maximus is frequently atrophied whereas the superior gluteus maximus is hypertrophied and tight. The hamstrings may be 'misused' to pull the body forward across the foot. This may result in excessive posterior pelvic tilt, which may make a person appear to be 'sitting down' whilst running. When the hamstring pull is unilateral then a shear force of the ilium on the sacrum may occur. The hamstring muscles are often short and weak suggesting that stretching would result in some instability of their 'energy strap' function. Moreover, during the transition from eccentric to concentric contraction if a muscle is too short then inefficient use of it's elastic recoil potential energy occurs. Therefore the muscle may need to be long and strong in a functionally specific manner.
The Iliopsoas muscle is used to pull the body forward over the stance leg during fast running. The Psoas Major has a different timing of contraction to the Iliacus during jogging compared with walking suggesting that the Iliacus acts as a stabiliser during slower activity. Furthermore, the iliacus is an anterior rotator of the ilium whereas the Psoas Major is a posterior rotator of the ilium. Evidence exists to suggest that the posterior medial aspect of the Psoas Major may have a stabilising function whilst the lateral aspect may have a predominant mobilising role. Additionally, the Iliacus may be synergistically contracting with the lateral rotators of the hip to attain hip stability. Therefore, low threshold loading of slow twitch endurance muscles function to stabilise joint segments. Conversely, the laws of 'inverse dynamics' suggest that, the superficial 2-joint high threshold fast twitch glycolytic muscles act as 'energy straps' transferring forces from one body segment to the next (Power = force x velocity) Thus, anterolateral part of the Psoas Major may be considered as a mobiliser whereas the iliacus may be considered a stabiliser. Since the rectus femoris is the only quadriceps muscle which crosses both the knee and hip then it can also act as an 'energy strap'. Importantly, if the muscle becomes short it may lose some of it's potential recoil energy during the transition from eccentric to concentric contraction ( see foot orthotics elsewhere on this site for an example ).
Any stiffness in the rectus femoris muscle can create anterior rotation of the ilium resulting in shear across the sacroiliac joint, as well as potentially creating excessive extension and rotation in the spine. The deep stabilising muscles of the spine and abdominal region will have to work exceptionally hard to prevent excessive and unwanted movement. Thereby, inefficiency in running and walking economy may occur (see running section for further details ).
Notably, the larger muscle groups can have differing functions. For example, the gluteus medius has an anterior, middle and posterior aspect and therefore can create vectorial forces from each of these directions. Additionally, at least 2/3rds of a muscle's longitudinal tension can be dissipated in the muscle's transverse direction. Finally, it must be emphasised that most muscles have a glycolytic and oxidative capacity whose proportions are genetically determined, but whose transitional fibres can mutate depending upon the type of metabolic demand the exercise prescription entails. Taken together, it is highly likely that the most effective exercise prescription is functionally specific to the goals of the task which is being rehabilitated.
Altered breathing patterns during lumbopelvic motor control tests in chronic low back pain: a case–control study
Nathalie Roussel, Jo Nijs, Steven Truijen, Liesbet Vervecken, Sarah Mottram, and Gaëtane Stassijns
Abstract
The objective of the study was to evaluate the breathing pattern in patients with chronic non-specific low back pain (LBP) and in healthy subjects, both at rest and during motor control tests. Ten healthy subjects and ten patients with chronic LBP participated at this case–control study. The breathing pattern was evaluated at rest (standing and supine position during both relaxed breathing and deep breathing) and while performing clinical motor control tests, i.e. bent knee fall out and active straight leg raise. A blinded observer analyzed the breathing pattern of the participants using visual inspection and manual palpation. Costo-diaphragmatic breathing was considered as optimal breathing pattern. Subjects filled in visual analog scales for the assessment of pain intensity during the tests. At rest, no significant differences were found between the breathing pattern of patients and healthy subjects (P > 0.05). In contrast, significantly more altered breathing patterns were observed in chronic LBP-patients during motor control tests (P = 0.01). Changes in breathing pattern during motor control tests were not related to pain severity (P > 0.01), but were related to motor control dysfunction (P = 0.01).
Inspiratory Muscle Training has been shown to improve proprioception (sense of joint position) in people with low back pain
In a previous investigation it was shown that individuals with recurrent nonspecific low back pain (LBP) and healthy individuals breathing against an inspiratory load decrease their reliance on back proprioceptive signals in upright standing. Because individuals with LBP show greater susceptibility to diaphragm fatigue, it is reasonable to hypothesize that LBP, diaphragm dysfunction, and proprioceptive use may be interrelated. After 8 wk of high IMT, individuals with LBP showed an increased reliance on back proprioceptive signals during postural control and improved inspiratory muscle strength and severity of LBP, not seen after low IMT. Hence, IMT may facilitate the proprioceptive involvement of the trunk in postural control in individuals with LBP and thus might be a useful rehabilitation tool for these patients. (Lotte et al, Medicine & Science in Sports & Exercise:January 2015 - Volume 47 - Issue 1 - p 12–19)
Habituation of the early pain-sensitivity respiratory response in sustained pain.
Kato et al (2001) Pain, 91, 57 - 63
Respiratory rate appears to be habitually high in the chronic pain state (from 13.2Hz to 17.7Hz)
- the pre Boetzinger brainstem complex appears to be the target for pro-nociception and anti-nociception input
- this may be significant in terms of the scalene muscles and thoracic outlet syndrome, thoracic spine posture and mobility; or in the case of diaphragmatic breathing, the lumbothoracic stability and rhythm
- additionally, alterations in sympathetic nervous system activity may be expected
Expertise in sport - what can be learnt from appropriate feed-forward mechanisms?
Expertise in sport is obtained through repetitive practice and the avoidance of injury. Where injury does take place appropriate recovery must follow. Often recovery was considered synonymous with being painfree. However, many recurrent conditions have been shown to be the result of ongoing motor dysfunction. Examples of gaining expertise and avoidance of injury using higher level motor programming and feed-forward mechanisms to evaluate relevant information
is discussed in the Orienteering section of this website .
see also Motor control of the cervical and lumbar spine
Conclusions
Inconsistent findings on the effects of pain on motor control has made it important to conceptualize a theoretical framework of adaptation in the sensorimotor system in the person with pain. A simplistic approach would be to say that the person will use the redundancy in the system to protect the perceived vulnerability to further injury. Such redundancy takes the form of employing synergistic muscles to perform the task and/or adapting the task to reduce loading. In the acute phase of an injury, such simple strategies may be useful, however adapatation can be very rapid and permanant. If the adaptation is suboptimal for the intended goal, then secondary injuries may occur. These may take the form of disuse atrophy, reduced sensorimotor (proprioceptive and feedforward) input from the 'unloaded' part, whilst overloading the compensatory muscles and the body parts which they influence. Therefore, both the primary and secondary consequences of the movement dysfunction must be evaluated and treated. Henry Tsao at the University of Queensland has quite clearly shown alterations in cortical processing regions (motor maps) in the brain in people with chronic low back pain. Adaptation strategies vary between people with both increases and decreases in muscle activity occuring in various parts of the body. Thus it becomes imperative that the person is examined in a systematic way in order to specifically taylor treatment management strategies.
Clinically, the examination process must ascertain the affect of pain and injury on attention and stress and its affects on the interpretation of task demands and hence motor planning. The effects of cortical inhibition, delayed central transmission, reflexogenic motoneuron inhibition on motor planning can lead to an altered internal model of body dynamics. Clinically this may manifest as reduced range of motion, altered reflexes and muscle strength, as well as changed movement goals to protect the body part. The clients perception of their problem is a vital part of a 'top down' approach to assessment and treatment. A 'bottom up' approach views the adaptive mechanisms in terms of altered proprioceptive input resulting in inaccurate motor planning. For this reason combination therapy, using passive modalities such as joint mobilizations, taping, dry needling, soft tissue massage, etc must be accompanied by meaningful and well integrated exercise prescription which takes into account the values and beliefs of the client. Moreover, in some cases a real and/or virtual exercise regime may mean that passive modalities are either unwarranted or contraindicated. Cognitive Behavioural Therapy may be required to address the aspects of 'attention' and 'stress'. "Mindefullness" may be another approach which could be undertaken. Regardless, of the approach taken, the goal should be to educate the client on their condition and how treatment interventions can meet and enhance their expectations.
"It is the thoughts which preceed the action which count
considered thoughts, considered action
decisive thoughts, decisive action
constructed thoughts, constructed action"
Later stages of exercise. Once the low grade muscle stabilisations of the inner core, diaphragm and pelvic floor have achieved adequate IAP (intra abdominal pressure) in varoius low load functional movements such as sitting, sit-to-stand, one leg stance, etc, some more dynamic stabilisation procedures may also be applied. However, it should be noted that high threshold stabilisation is not a replacement for low grade stabilisation. These are two completely different exercise regimes where in fact too much Global Ballastic muscle activity will inhibit low threshold endurance stabilising capacity.
Remember 'stability means controlled movement' also see Clinical Instability of the Lumbar Spine
Non linear mechanics
Joint Hypermobility
Joint Hypermobility and Ehler Danlos Syndrome
Excessive weight can also compromise the efficiency of movement and create excessive loading of musculoskeletal structures.
Exercise and weight loss is discussed elsewhere in this website.
Psychology
Psychosocial and Cognitive Factors in Pain
Brain imaging of pain
Training methodology
Madelaine P (2008) Functional adptations in work-related pain conditions. In Fundamentals of Musculoskeletal Pain, Graven-Nielsen & Arendt-Nielsen Eds, IASP Press Seattle Ch 25
Moseley GL & Hodges PW (2006) Reduced variability of postural strategy prevents normalization of motor changes induced by back pain: a risk factors for chronic trouble? Behav Neurosci, 120, 474 to 476
Last update : 17 October 2020