Achilles Tendinopathy - clinical reasoning, pathological and biomechanical perspective in physiotherapy
by Martin Krause
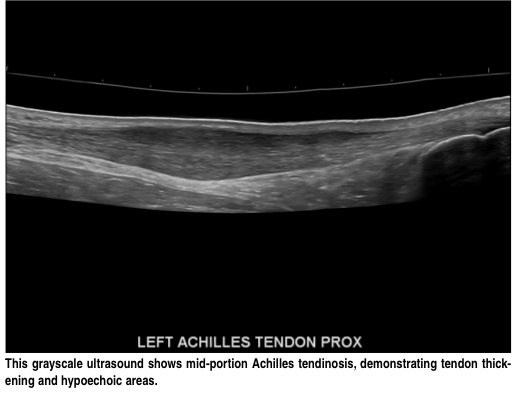
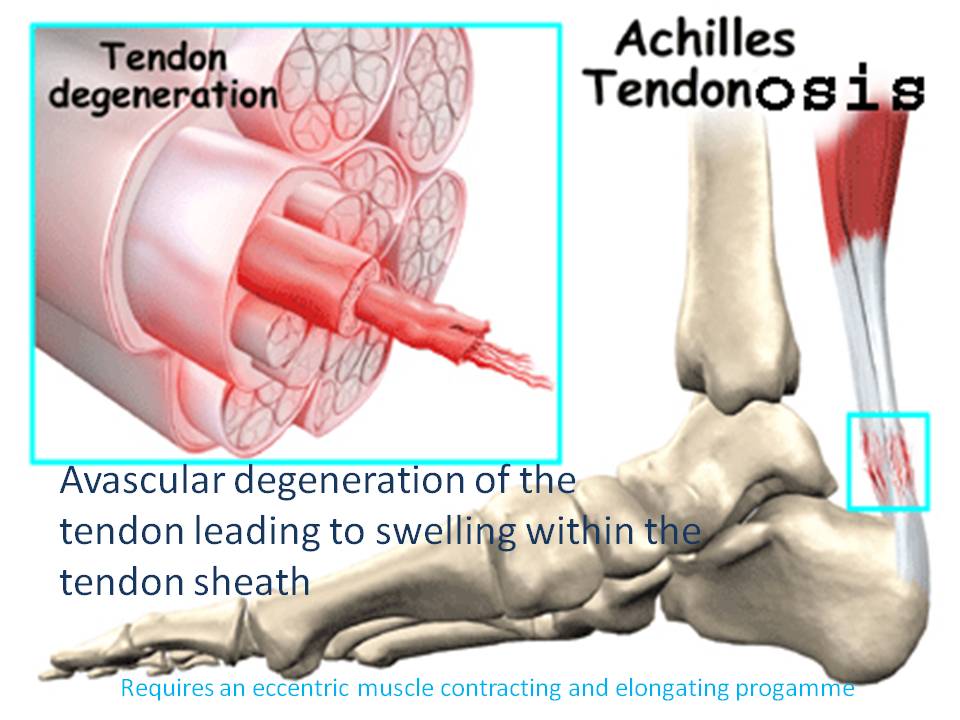
The Achilles tendon is a thick strong mass of avascular collagen fibres who attains it's nutrition through the process of diffusion of nutrients down a pressure gradient. Achilles injuries are usually classified into acute tears and paratendonosis. The latter occurs frequently in males over the age of 40, whose high testosterone and reduced chondroitin-6-sulphur levels mean that their collagen matrix has become drier and more brittle. Ironically, these people can present with swelling in the mid substance of the tendon due to neovascularization of the tendon. In contrast, acute ruptures of the tendon can occur at any age, and hence these people may present clinically with complete rupture of the Achilles substance from the bone, mid tendon or musculotendonous junction ruptures. It commonly occurs in sprinting and jumping sports where fast changes in muscular lengthening and shortening occur. People with large tight calves and those with a pes cavus (high arched) foot are at greater risk of getting such a tear. On the other side of the coin, are the people with long flattened arches which make them slow and/or weak in their supination component of push-off. These people frequently develop a mid medial calf tear. Over-active lateral gastrocnemius and underactive soleus have also been implicated as has excessive eversion of the ankle during the stance phase of gait. Finally, some people have a very low insertion of their deep calf muscle (the soleus) on the Achilles making the tendon inherently shorter. Complete and partial tears are treated with camwalker boots, complete immobilsation or surgery with or without autologous grafts such as using the plantaris tendon. Additonally, to Achilles tendon problems are insertional problems on the heel associated with an inflammed (calcaneal) bursa. These tend to have a metabolic - immune compromise and may have a direct mechanical irritation from a lateral (outside) calcaneal spur (Haglunds exostosis). These latter conditions tend to prefer a heel raise and don't necessarily do well with heel drops as an exercise rehabilitation regime. The gut biome needs to also be addressed in bursitis conditions. Further differential diagnosis needs to be made with an Os Trigonum (posteromedial bone formation with the foot-big toe flexor).

Harglunds Exostosis (deformity) - above and below

Os Trigonum - below

Chronic swelling inside the tendon sheath can lead to severe pain. Depending upon pathology a necrotic area of degeneration within the tendon may occur with concommittant blood vessel infiltration leading to further pain and swelling. Other factors leading to a potential Achilles problem also include myofascial-immune pathology, metabolic-immune-bursa pathology, and low back pathology (L5/S1 intervertebral disc), the latter resulting in neurologically generated tightness and weakness in the muscles of the calf and ankle. Additionally, people with chronic lateral ankle instability also seem to be at risk of Achilles tendonopathy (AT). In fact, the inverse dynamics of energy transfer, where muscles crossing 2 joints are seen as energy straps, implicate the entire lower limb in Achilles pathology.
Researchers found the impulse of the hip adduction and external rotation moments as well as the peak hip external rotation moment to be significantly increased in runners with AT compared with their healthy counterparts (Creaby et al 2017, Med Sci Sp & Ex 49, 3,:549-554), However, the two groups displayed similar hip and ankle joint angles as well as ankle joint moments during running. The identified differences in hip joint biomechanics found in this study compliments previous research that provided evidence of altered hip neuromuscular control in runners with AT (Azevedo et al, Br J Sports Med. 2009;43(4):288–92; Franettovich Smith et al, 2014 Med Sci Sp Ex. 46 3, 594–9). Taken together, these findings reinforce the need to consider proximal lower-limb function in the assessment and rehabilitation of runners with AT.
Index
The kinetic chain
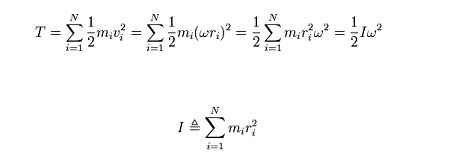
The Achilles tendon forms part of a kinetic chain of accelerating levers (bones) around which energy is transfered and dissipated through lengthening (eccentric) and shortening (concentric) contractions between the foot and thorax.
Inverse dynamics in an accelerating lower limb include the capture and release of kinetic energy through the conservation of angular momentum.
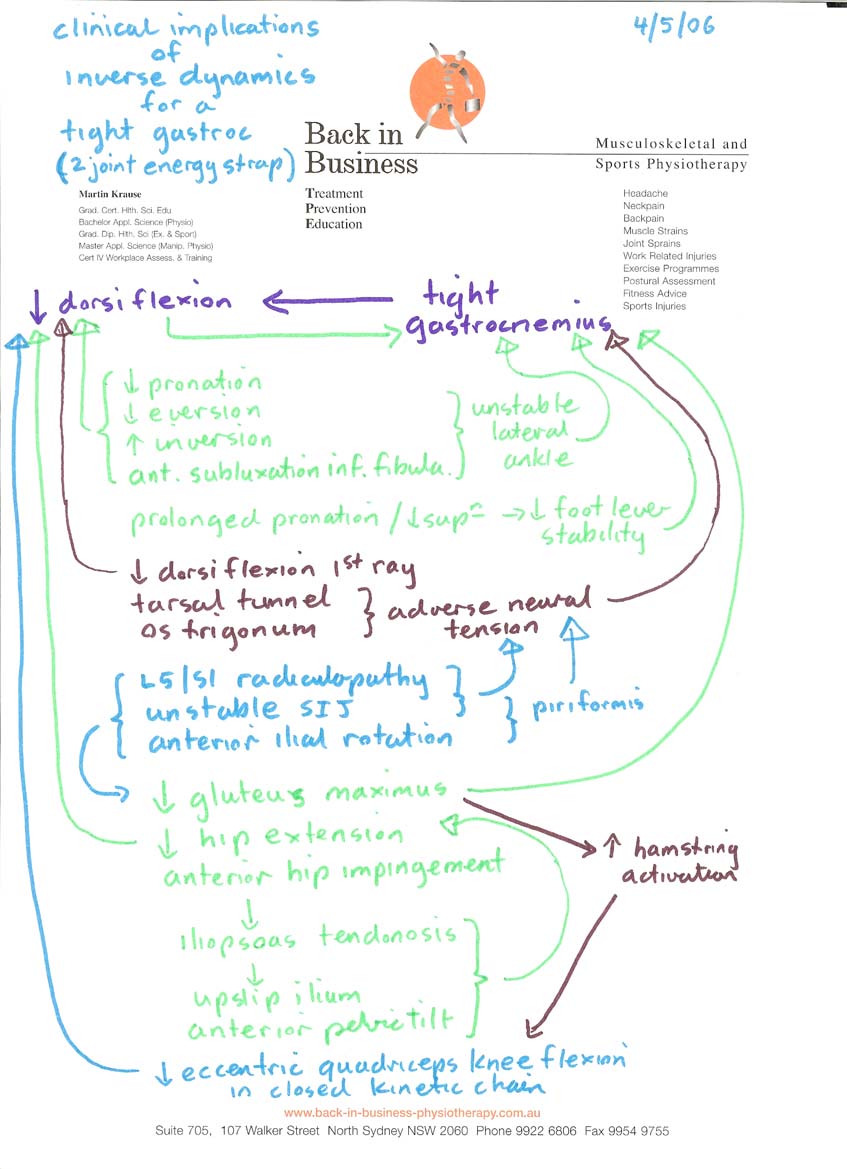
Clinical implications of inverse dynamics - chronic ankle instability
Tendons act as buffers, delay energy absorption by muscles and hence act as attenuators and shock absorbers and thereby have implications for neural control (Roberts & Konow 2013, Ex Sp Sc Rev, 41, 4, 186-193). If tendons are injured, or if a pain state exists the ability to engage the elastic components of movement is diminished. In fact, people with chronic ankle instability (CAI) have been shown to have decreased energy dissipation at the knee during jumping (Terada et al 2013, Med Sc Ex Sc, 44, 11, 2120-2128). Additionally, people with CAI demonstrate reduced ankle and knee torques with concomittant increases in hip torque during jumping and landing activity (Kim et al 2018, Med Sc Sp Ex, 50, 2, 308-317). Hence, CAI potentially makes those people more likely to have injuries to the knee, hip and spine through altered distribution and dissipation of load. Mind maps can be generated which illustrate the multifactorial nature of calf tightness and achilles pathology. It should be noted that this 'mind map' was generated 7 years before researchers vindicated the use of such an approach. This is a 'classic' example whereby clinical reasoning can define the treatment rationale even in the abscence of evidence based physiotherapy (EBP). In this case, the amelioration of clinical signs and symptoms provides the face and construct validity to drive the EBP, where the 'mind map' is a construct from a combination of energy transfer biomechanics and clinical reasoning.
Neuroplasticity in tendinopathy
A multitude of contributing factors to altered motor control must be addressed when treating tendon dysfunction. What we have failed to consider in the past when dealing with chronic or recurrent tendon issues are motor control problems encompassing corticospinal control of excitation and inhibition as well as belief systems about pain and contextual factors related to imaging.
Research by Ebonie Rio et al (2015) (BJSM Sept 25, 10.1136/bjsports-2015-095215) suggest that the pain state sets up an adaptive pathway whereby the ipsilateral kinetic chain is directly inhibited by reflexogenic pathways, as well as being inhibited by contralateral hemispheric activity. Simultaneously excitation is enhanced in the opposite limb as well as in antagonists...at least in the case of enhanced excitation of the hamstrings in quadricep tendinopathy. If this is true, then so much for training the contralateral limb for 'cross training' purposes! Furthermore, they recommend enhanced corticospinal drive through the use of 30-60 second isometric holds at 70-80% MVC to load the muscle whilst using isokinetics to load the tendon. Moreover, they recommend the use of a metronome at 60bpm (stages 1 and 2) with a count of 3 up, 2 down for quads, and 2 up, 3 down for calf isokinetics to optimally engage corticospinal drive through the visual and auditory stimuli (also shown by Kohei et al 2012 {Int J Rehab Res, 35, 1, 82-84} for motor imagery and M1 stimulation).
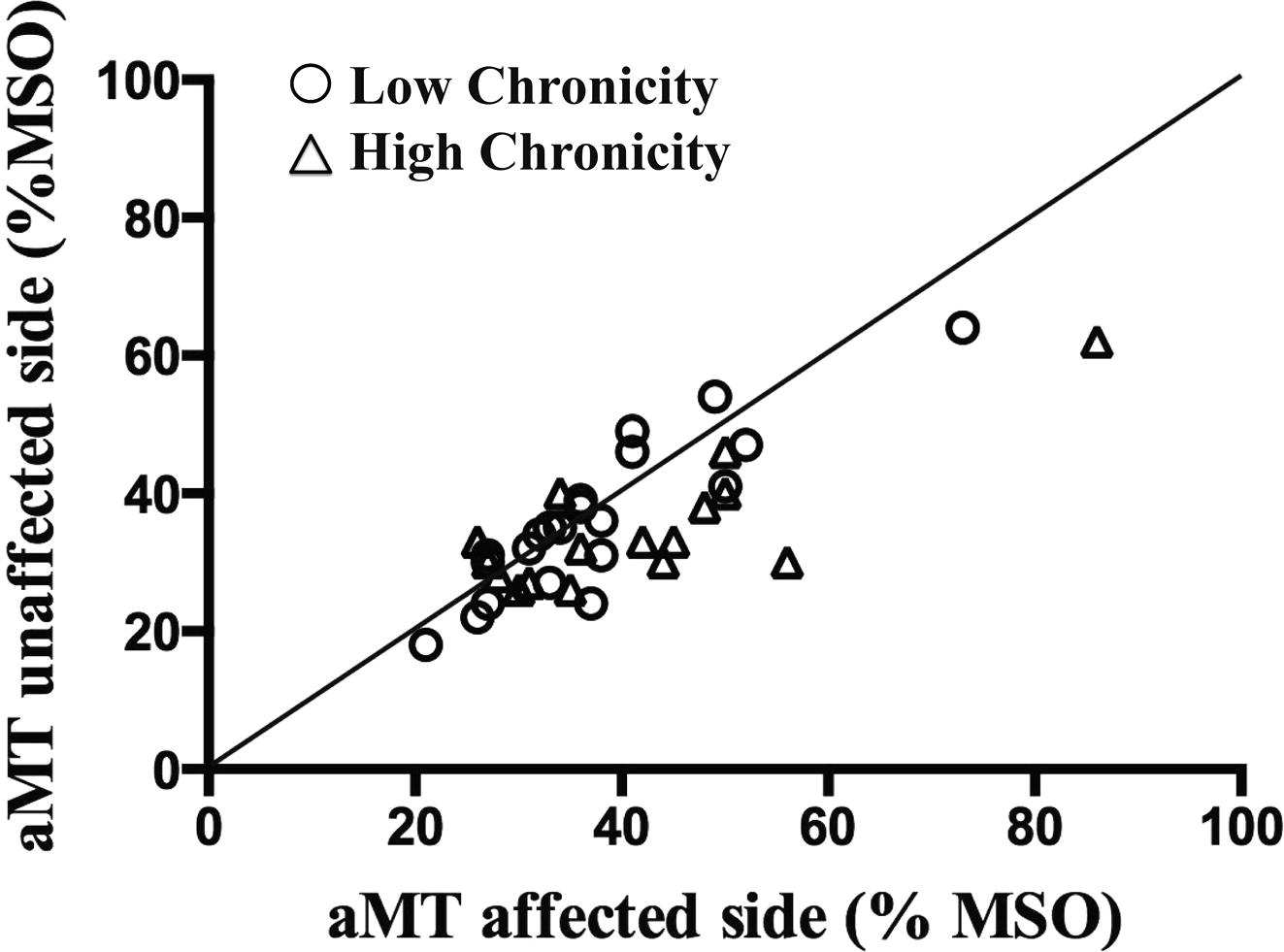
Cortical mapping of infraspinatus muscle in chronic shoulder pain demonstrating higher motor thresholds (aMT= activation MT) and hence reduced excitability on the affected side (39 vs 35) (Ngomo et al 2015 Clinical Neurophysiol, 126, 2, 365-371)
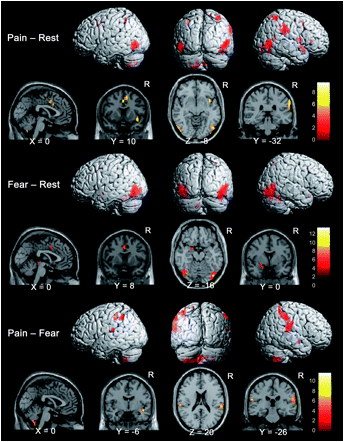
Cortical mapping of pain and fear. Lots of overlap suggesting that taking away the fear from the pain with good clinical explanations and a focused goal directed program with specific functional outcomes are important.
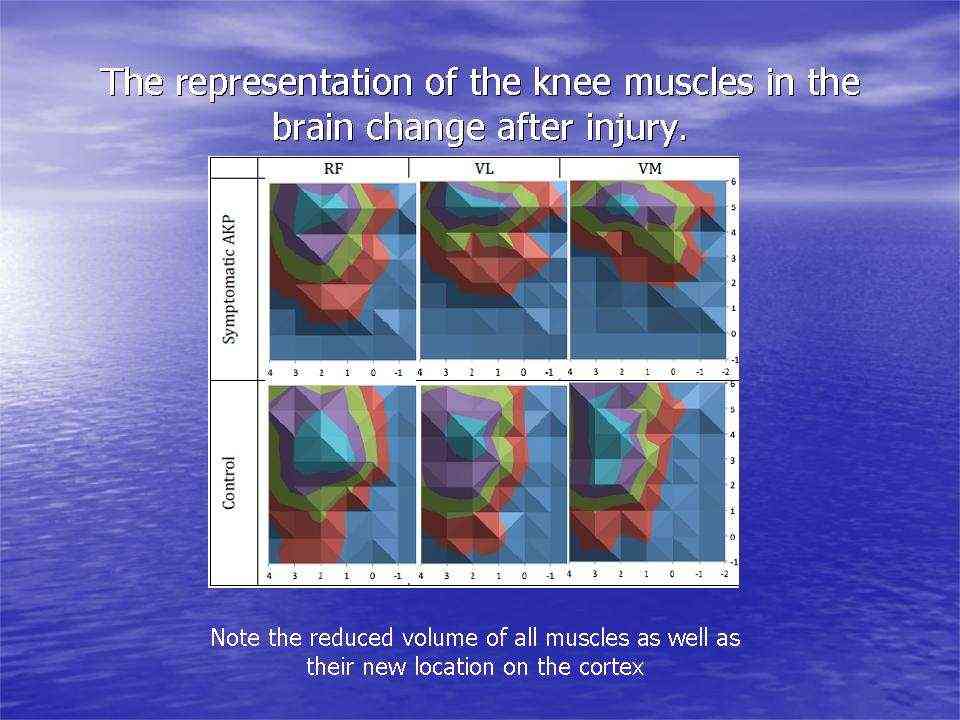
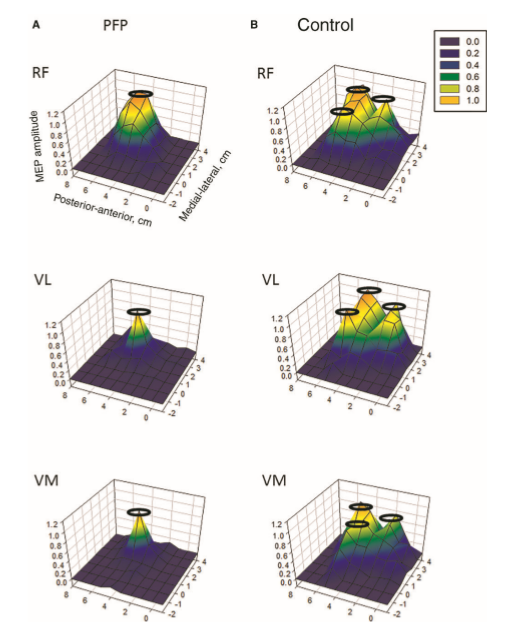
Individuals with patellofemoral pain (PFP) had reduced map volumes and an anterior shift in the M1 representations, greater overlap of the M1 representation and a reduction in cortical peaks across all three quadriceps (RF, VL, VMO) muscles compared with controls (Te et al 2017 Pain Medicine, pnx036, https://doi.org/10.1093/pm/pnx036).
By extrapolating from this work on knee pain and cortical representations, it appears highly probable that cognitive filtering and re-adaptation at a cortical level is essential for tendon recovery. Electrical muscle stimulation and isometric muscle contractions can be used to achieve such goals.
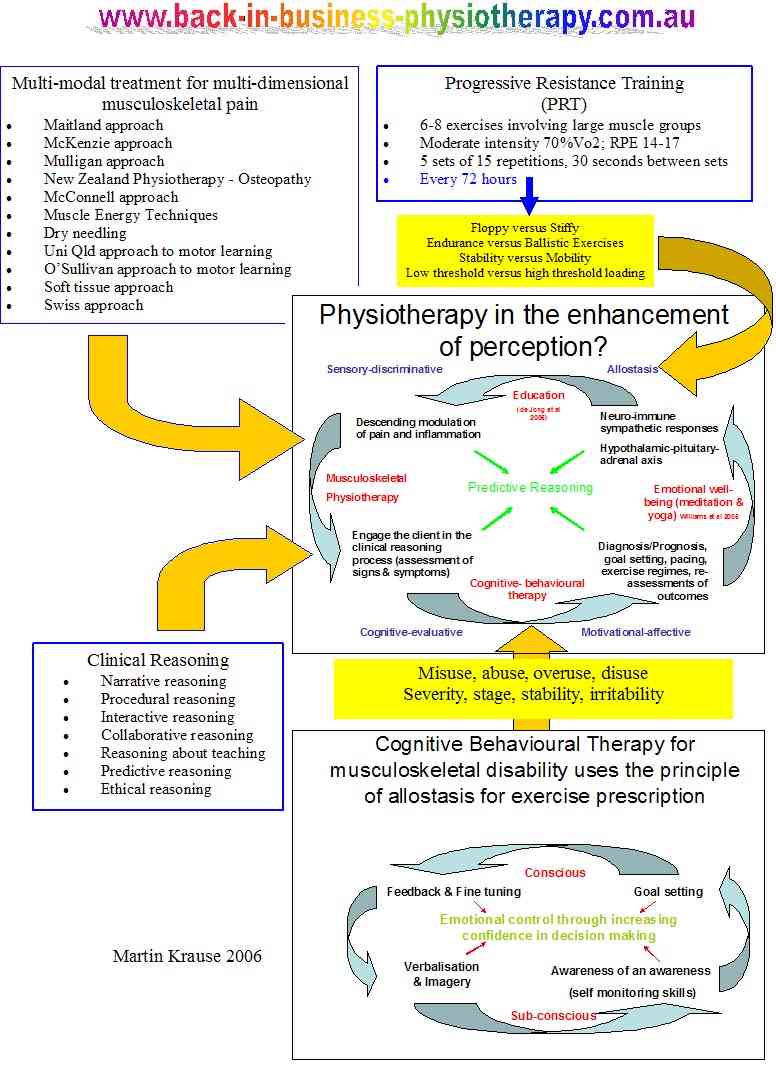
Cognitve filtering by the therapist
.Mind maps can highlight the need to develop a structured approach to treating an Achilles tendon problem. Multiple hypotheses testing requires a mechanism of filtering multiple information so that the clinical signs and symptoms can be integrated with knowledge from pathophysiology, which subsequently generates decision making and treatment strategies based on testable clinical pattern generation.
Refinement of the working hypothesis
All clinical findings (impairments measures) need to be assessed in relationship to the subjective examination (disability measures, past and current history w.r.t mechanism of injury/onset and/or aggravating/easing factors) in order to determine a diagnosis and prognosis based on the stage, stability, irritability and severity of the disorder. This process should also identify whether we are dealing with misuse, overuse, abuse or disuse as a precipitating factor in it's onset and/or chronicity. By defining the disorder into these categories the clinician is consciuosly 'filtering' the multitude of information to form a 'clinical picture'.
Multimodal approach to multifactorial dimensions of a problem
The clinical reasoning process is used to confirm and negate correlations between the multiple variables. These findings must then be integrated into the neuro-matrix to determine a management plan which encompasses the goals and asperations of the client.
Predictive reasoning
The ultimate goal for the musculoskeletal physiotherapist is to integrate the neuro-matrix into a clinically useful management strategy where predictive reasoning enhances the clients confidence in their therapist and in their own decision making processes
Treatment options
Treatment could consist of
- Camm walker boot
-
Dry needling, myofascial release & soft tissue massage
- Kinetic or dynamic taping
-
Foot - ankle taping, orthotics/heel raise
-
Muscle energy techniques for lumbar spine - SIJ dysfunction
-
Metabolic consideration - Mg-Ca, Na-K balance
-
Nutritional Considerations - protein-carbohydrate, creatine supplementation
-
Joint mobilisation to the foot, inferior and superior fibula, hip, sacrum & lumbar spine
-
Functional closed chain oscillatory eccentric - concentric exercises for lumbar spine, hip, knee and ankle
- Neuroplasticity training using isometric and metronome driven isokinetic exercises

Exercise progression to incrementally load the Achilles tendon
An interesting biomechanical analysis, using force platforms and kinematic (3D motion analysis) data compared Achilles tendon loading during various activities, they were able to develop an loading index (Baxter JR et al 2021 Med Sc Sp Ex, 53, 1, 124-,130). They found that during walking at 1.5 m/s, tendon loading was 3.7 body weight (BW), during self selected running speed 6.3 BW (loading impulse 0.8 BW/sec), counterweight movement jump 3.4 BW, double leg hop 4.8 BW. Such information is incerdibly useful when designing a rehabilitation programme appropriate to the stage of recovery.
Lateral ankle instability contributing to a Achilles tendonopathy
If lateral ankle instability is accompanied by calcaneal valgus during mid stance (foot flat phase), then the medial aspect of the achilles is lengthened greater than the lateral aspect, creating torsion within the tendon. Subsequently, such torsion results in weakened push off and paradoxically excessive calcaneal varus on heel raising, reversing the medial-lateral lengthening and tension relationship within the achilles. Therefore, ankle instability needs to be addressed in the management of Achilles Tendinosis.
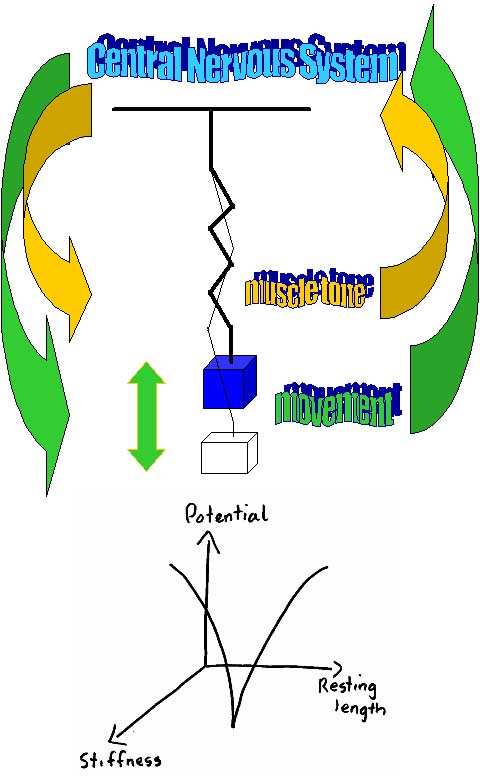
Motor control of countermovement jumps
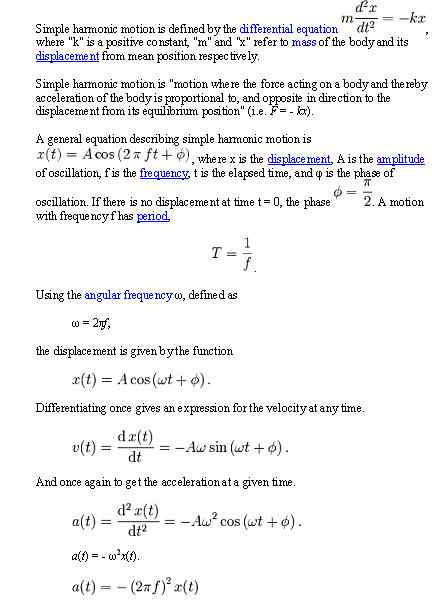
Countermovement jumps have been demonstrated to improve with eccentric Achilles tendon loading. Neural modulation of the muscle -tendon control strategy was shown to change after 1 bout of practice. These changes included a decrease in the magnitude of fascicle lengthening and shortening, which was accompanied by an increase in tendon shortening without a change in ankle ROM (Hirayama et al 2012, Med Sc Sp Ex, 44, 8, 1512-1518). Motor control suggests that the 'degrees of freedom' are controlled using a mass spring analogy of oscillations around a point of CNS stability. This stability is based on the balance of muscle tone as well as predicted feedforward movement oscillations.
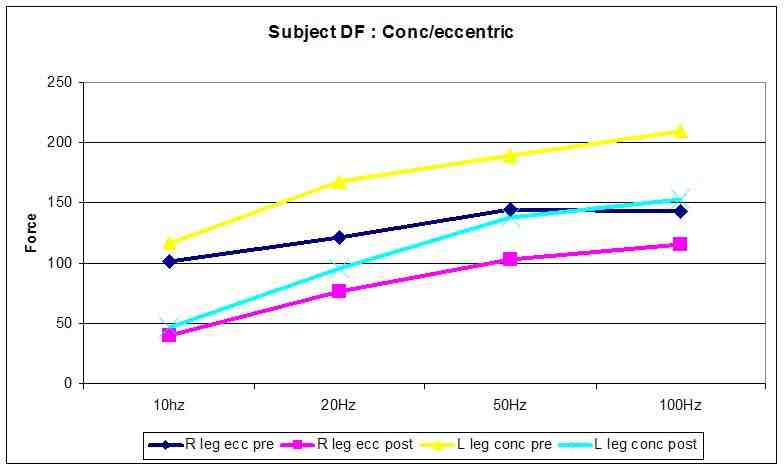
Plyometrics and eccentric muscle adaptation (Martin Krause 2003)
The eccentric component to this exercise cause more profound changes to the connective tissue of the muscle (broadening and streaming of Z bands). Investigations into eccentric exercise revealed pain 8 hours after initial exercise which was maximal 48 hours later (Newham, Mills, Quigley, Edwards 1983). These investigators found low frequency fatigue 10 minutes after a 20 minute period of stepping (Newham et al 1983). Additionally, they demonstrated progressive increases in IEMG during the exercise in the rectus femoris (160% increase) and vastus medialis (140% increase) in the eccentric contracting leg (Newham et al 1983). Mechanical damage to the sarcoplasmic reticulum resulting in less calcium release for each excitatory action potential was suggested as the cause of the low frequency fatigue (Newham et al 1983).
Muscles undergo fatigue and weakening after several bouts of concentric and eccentric exercise. Moreover, this fatigue and weakness is usually more extreme after eccentric exercise in the untrained individual. A number of sites in the myo-fibrillar complex such as reduce binding sensitivity and capacity of Troponin C for calcium, altered troponin-tropomysosin interaction to impaired binding and force generation by actin and myosin have been implicated in impaired force generation (Green 1990). Indeed, in the absence of any association between relaxation rates and Calcium kinetics raises support for the notion of a rate-limiting process controlling the relaxation of fatigued muscles being located in the contractile proteins (Hill et al 2001). During fatigue the relaxation times can be prolonged as much as 50% (Bigland-Ritchie et al 1986) thus resulting in increased force generation during sub-maximal stimulation due to tetanic fusion despite a substantial fall in the maximum tetanic force (Bigland-Ritchie et al 1986).
The initial overall loss of force production seen may be due to Desmin and Titan damage (Lieber & Friden 2002). Desmin acts as an extra-sarcomeric mechanical stabilizer between adjacent Z discs and the attachment to the costomere at the sarcolemma (Lieber, Shah & Fridén 2002). The costomere complex contains Talin, Vinculin & Dystrophin which attach to the trans-sarcolemmal proteins Integrin and Dystrophin associated proteins. These proteins allow the lateral transmission of force from actin to the basal lamina containing type IV collagen which is contiguous with the endomysium (Kovanen 2002). Desmin loss after eccentric exercise can occur within 5 minutes, possible as a result of increased intracellular Calcium leading to Calpain activation and selective hydrolysis of intermediate filament network (Lieber & Fridén 2002). This may result in the ‘popping of sarcomeres’ of different length may loose their myofilament overlap of actin and myosin (Lieber & Fridén 2002). Hence, reduced force production would be expected. Additionally, the release of matrix metalloproteinase (MMP) which may degrade the extramyocellular type IV collagen (Korskinen, Kovanen, Komulainen et al 1996). However, this effect occurs many days after exercise (Korskinen et al 1996) and could even effect torque production 28 days after exercise (Lieber & Fridén 2002). This has significant implications in exercise training prescription.
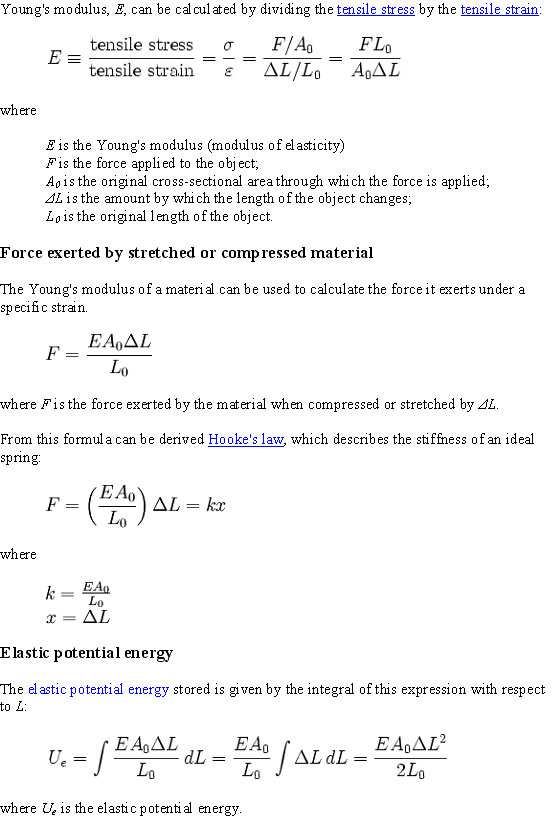
Tendon properties under loading
A meta-analysis of increased loading on in-vivo tendon propeerties (Wiesinger et al 2016, Med Sc Sp Ex,47, 9, 1885-1895) confirmed a nearly systematic change in tendon properties with training. The patella tendon appears more amenable to change than the achilles tendon in terms of tendon stiffness. A rapid increase in Young's modulus is often paired with tendon stiffening and remains elevated within the first months of trainng in a rather monotonic fashion, whereas long term, years of training was associated with a larger tendon cross sectional area, without any evidence of differences in material properties. Mechanisms of change include extracellular matrix (ECM) enzymes involved in collagen turn-over, such a matrix metalloproteinases. Furthermore, an up-regulation of the stress response cytokines and growth factors (insulin like growth factor or transforming factor-beta-one) have been observed in Acchiles tendons in vivo and patella tendons in vitro. It should be noted that isometric exercises do not load tendons to a great extent, whereas isokinetic eccentirc/concentric exercises do.
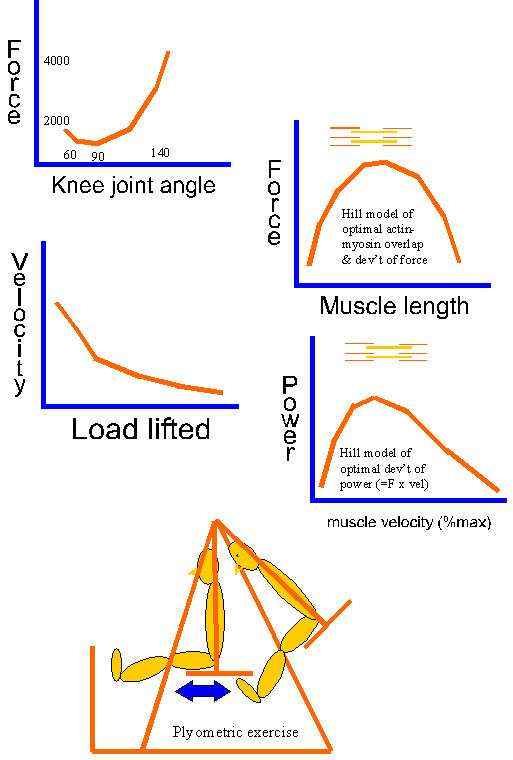
Is muscle injury the result of an imbalance between intra-muscular transverse and longitudinal forces?
Is muscle tightness due to an imbalance between force and velocity and hence the development of power? This highlights the need for specificity with training and rehabilitation.
Force damping and recoil leads to efficient transfer energy which in the case of walking has been related to sinusoidal movement. Longer lower limb tendons, especially the Achilles Tendon, and stiffer lower limb joints have been shown to lead to improved running efficiency (Hunter et al 2011, Med Sc Ex Sp, 43, 8, 1492-1499). Clinically, however, we need to differentiate between the 'floppies' and the 'stiffies' as tendon-muscle complexes can be long and stiff as well as short and stiff in individuals with strong collagen complexes versus those with weaker more pliable ones. Other investigators also found that six weeks of plyometrics training improved running performance and the ECR (energy cost of running) despite no measurable changes in MHC (myosin heavy chains) and titin isoforms. This plyometric intervention improved 3000m time trial performance and oxygen consumption. Plyometric training consisted of 15 sessions. The sessions included total contact time of between 60 to 228, and the intensity of vertical jumps increased progressively using a slightly modified Spurrs protocol to avoid injury. Vastus lateralis was used as a biopsy site. (Pellegrino et al 2015, Med Sc Sp Ex, 48, 1, 49-56). In my clinical experience, regardless of the site of lower limb tendonopathy, similar to principals of myofacial trains (eg deep myofascial train of the calf is continuous with underside of the patella), the entire kinetic chain needs to be treated and the plyometric exercise protocol should resemble sporting specificity. For example, soccer players should be able to do at least 3 sets of 30 heal drop/raises, 3 sets of 90 one leg bridging, 3 sets of 90 hip drop/hitches and 6 sets of 60 quads 'hover' eccentric/concentric activity.
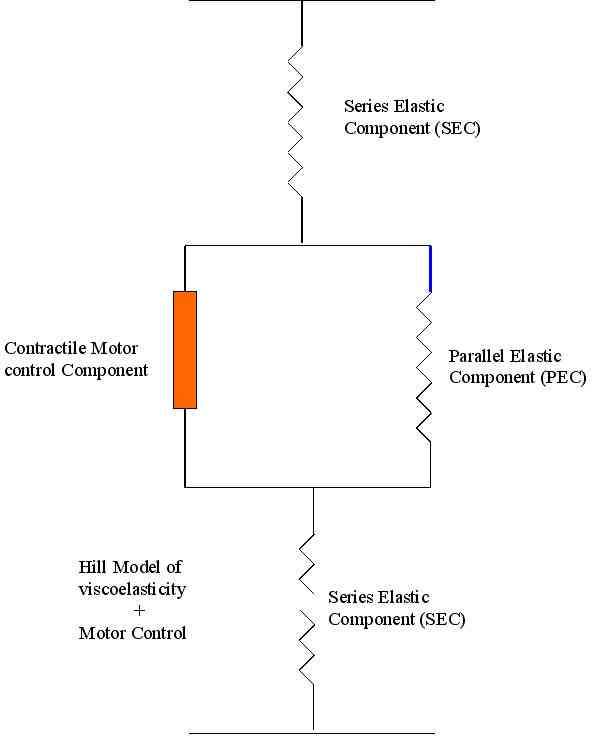
The concepts of Young's modulus of elesticity and the Hills Model of viscoelasticity should not be confused with the Mass-Spring Concept of motor control and Inverse Dynamics.
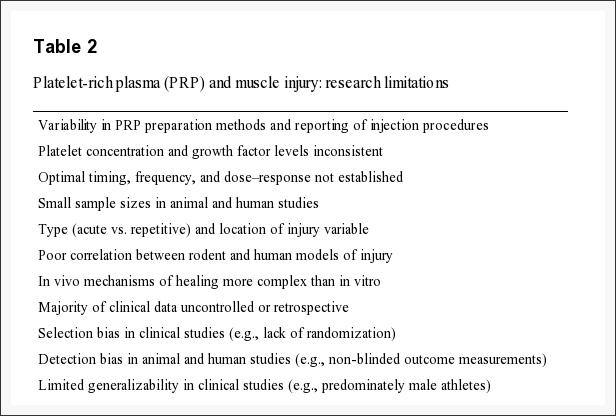
PRP
In vitro studies and animal research have suggested that PRP may have benefits associated with the increased release of cytokines and growth factors resulting from supraphysiological concentrations of platlets that facilitate muscle repair, regeneration, and remodeling. Despite the promise of basic science, there is a paucity of clinical data to support the theoretical benefits of PRP. The only double blind controlled clinical trial was shown to have no benefit of PRP in the time to resume sports activity among athletes with hanstring injuries (Mosca & Rodeo 2015 Current Rev Musck Med, 8, 2, 145-153).
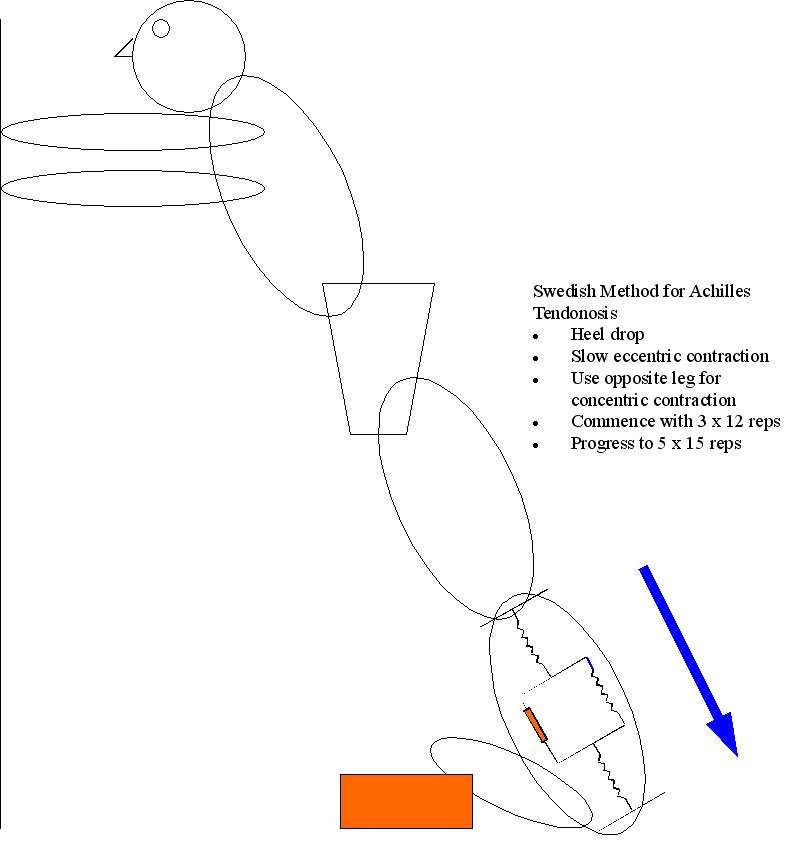
Conclusion : the Swedish method of treatment using eccentric calf loading for optimal collagen alignment
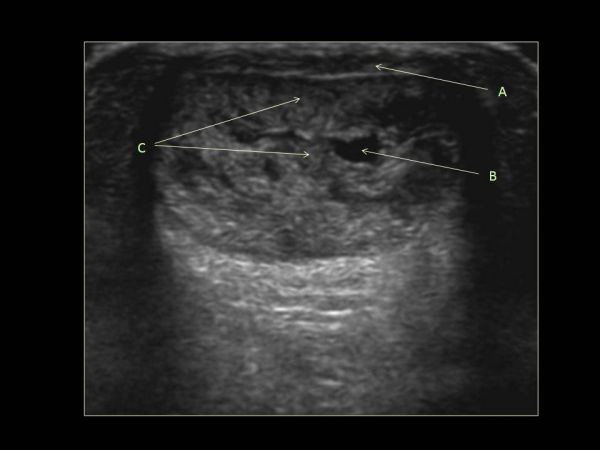
The Swedish method of rehabilitation for Achilles Tendinosis has used the concepts of eccentric loading to propogate nutrition to the muscles, encourage lengthening of the actin-myosin resting position as well as improve viscoelasticity through enhanced collagen turnover. Thereby, a mechanical input is transduced to a cellular response. However, Achilles tendinopathy has an aberrant strain response to eccentric exercise. Researchers concluded that Achilles Tendinosis is a bilateral systemic process where they found that both the symptomatic and asymptomatic tendons were thicker and hypoechoic when compared with control tendons. Furthermore, they showed altered fluid movement within the tendon matrix which was characterized by lower acute anteroposterior response to eccentric exercise (Grigg et al 2012, Med Sc Sp Ex, 44, 1, 12-17). Moreover, human muscle proteome modification after acute or repeated eccentric exercises is towards a switch to an oxidative metabolism (Hody et al 2011, Med Sc Sp Ex, 43, 12, 2281-2296), which suggestive of protection against DOMS as well as a progenetor for recovery and repair.
The science behind a 12 week eccentric training for Achilles Tendonosis are an increase in collagen synthesis (Langberg et al 207) and reduced neovascularization (Ohberg et al 2004) leading to reduced capillary engorgement and improved venous return (Knobloch et al 2007). These latter authors demonstrated a 45% improvement in capillary blood flow and reduced pain on a VAS after a 12 week eccentric training progam. Furthermore, Webborn (2008) suggested that clinical improvements were also related to nerve blood flow issues coined "neoneurovascularization". It should be noted, however, that this method might not be appropriate if the retro-calcaneal bursa is involved. Generally, to differentiate a tendonosis from a bursitis, the area of swelling is in the mid substance of the tendon for tendonosis, whereas it's at the insertion for bursitis. Remember, bursitis is a metabolic - immune reaction and probably wants to be unloaded with a heel raise and treated with voltaren-hirudoid or arnica wrap, whereas mid substance tendonosis prefers to be loaded in the manner described here. Not with-standing para-tendonitis also enjoy the wraps. None of these conditions like to be irritated by footware -so choose wisely.
http://youtu.be/FiIrYG0p5qQ
Achilles tendon stiffness has been shown to increase with plantar flexion training by between 16% and 29% (Kubo & Ikebukuro 2012 Med Sc Sp Ex, 44, 11, 2111-2117). However, these values are lower than increases of between 58% and 83% in patella tendon stiffness after knee extensor training. These results, in line with previous comments, suggest a difference in the plasticity of the two tendon types. Furthermore, sprinters appear to have a more elastic patella tendons, whereas endurance runners had stiffer patella tendons when compared to lesser trained individuals. These differences appear to be the result of higher blood flow in the patella tendon when compared with the achilles tendon (Kubo & Ikebukuro 2012). Improvements in blood flow to the Achilles tendon was only shown after repeated contractions of 70% MVC whereas 50% MVC showed no change in perfusion. Furthermore, these investigators demonstrated improvements (7.7%) in achilles tendon perfusion (total haemoglobin and oxygen saturation) from 20 minutes of heating using a hot pack. The generalised reduction in Achilles perfusion when compared to the patella tendon may partially explain the greater propensity to rupture achilles tendons.
A multitude of contributing factors to altered motor control must be addressed when treating tendon dysfunction. What we have failed to consider in the past when dealing with chronic or recurrent tendon issues are motor control problems encompassing corticospinal control of excitation and inhibition as well as belief systems about pain and contextual factors related to imaging.
Research by Ebonie Rio et al (2015) (BJSM Sept 25, 10.1136/bjsports-2015-095215) suggest that the pain state sets up an adaptive pathway whereby the ipsilateral kinetic chain is directly inhibited by reflexogenic pathways, as well as being inhibited by contralateral hemispheric activity. Simultaneously excitation is enhanced in the opposite limb as well as in antagonists...at least in the case of enhanced excitation of the hamstrings in quadricep tendinopathy. If this is true, then so much for training the contralateral limb for 'cross training' purposes! Furthermore, they recommend enhanced corticospinal drive through the use of 30-60 second isometric holds at 70-80% MVC to load the muscle whilst using isokinetics to load the tendon. Moreover, they recommend the use of a metronome at 60bpm (stages 1 and 2) with a count of 3 up, 2 down for quads, and 2 up, 3 down for calf isokinetics to optimally engage corticospinal drive through the visual and auditory stimuli (also shown by Kohei et al 2012 {Int J Rehab Res, 35, 1, 82-84} for motor imagery and M1 stimulation).
Jill Cook, Ebonie Rio, Craig Perdam and Sean Docking (2017) suggest differentiating between a tendinosis and paratendinosis - the latter helped by a mixture of hirudoid and voltaren gel wrapped in clingwrap at night for 1 week during the acute phase, or in my experience make the wrap for exercise/movement during the day in less severe cases. Care needs to be taken that the latter approach isn't used just to mask the symptoms. Post exercise reductions in swelling and tenderness should occur. In contrast, tendinosis, as eluded to previously, requires an isometric program, where in the acute and subacute phases care is taken to avoid compression of the bursa (for the AT that's in dorsiflexion, for the PT it's in flexion). Furthermore, these reasearchers don't believe in injecting anything into a tendon. They also don't like the eccentric "Achilles heel drop' programme as they feel it places too much compression on the bursa-tendon complex. However, it may be a case of 'horses for courses' whereby the clinical reasoning process dictates the most appropriate intervention based on the stage, severity, irritability and stability of the problem. It's this authors opinion that, the parallel elastic components of the kinetic chain are of equal importance and thereby the solution may be a happy median, where in the acute and subacute phases eccentric programmes are avoided or reduced in their range of (compressive) motion, whilst being employed in less severe cases (functional impairment) or at later stages of the rehabilitation process.
References
Knobloch K et al (2007) Eccentric training decreases paratendon capillary blood flow and preserves paratendon oxygen saturation in chronic Achilles tendinopathy. Journal Orthopeadic Sports Physical Therapy, 37, 5, 269-276
Kubo K, Ikebukuro T (2012) Blood circulation of Patella and Achilles tendons during contractions and heating. Med Sc Sp Ex, 44, 11, 2111-2117
Langberg H et al (2007) Eccentric rehabilitation exercises increases peritendinous type I collagen synthesis in humans with Achilles tendinosis. Scandinavian Journal Medicine Science Sports, 17, 3, 298-299.
Webborn ADJ (2008) Novel approaches to tendonopathy. Disability Rehabilitation, 1-6.
See links to
Last update : 21 July 2021