Everyone knows that skiing requires strong control of the knee through the thighs. Frequently, people equate knee control with quadriceps strength and balance. Importantly, this balance isn't just the balance between inside (vastus medialis) and outside (vastus lateralis) strength, but also the balance between the hamstrings and quadriceps.
The bending and straightening component of the knee is certainly under the control of the hamstrings and quadriceps, however, the medial and lateral control of the knee is controlled by the muscles around the hip and foot. As such, the muscles around the hip and talo-navicular joints perform the function of multidimensional stability.
Clearly, the femur affects knee positioning and the position of the ilium/hip will affect timing of the muscles around the hip-thigh. Any anterior ilial rotation generally makes it difficult for the gluteus maximus to fire before or simultaneously with the hamstring muscles. Tightness of the adductor muscle can cause an 'inflare' of the ilium, potentially placing adverse tension on the ischiococcygeal and sacrotuberal ligaments. Moreover, this adverse tension of the adductors could affect the knee through the phylogenetic link of these muscles with the medial collateral ligament and hence medial meniscus. Any adverse function of the iliopsoas can affect femoral blood flow which is likely to affect slow twitch, stabilising, endurance muscles more than fast twitch, glycolitic, ballistic muscles. Hence, as the duration of activity increases, movement stability may break down, leading to 'poor form' and potential injury.
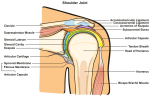
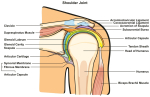
link to explanation in Shoulder section
Motor learning theory devised by Bernstein suggests that the body will use the momentum of the limbs to optimize the degrees of freedom in the system. Similar to a mass-spring analogy where the perturbations of the mass will be dependent on the damping characteristics of the spring, the brain will introduce muscle tone to dampen the angular velocity and hence acceleration of the system. Therefore, instead of the muscles of the leg lifting the limb, the antagonistic muscles are decelerating the limb towards the end of trajectory. Moreover, by using eccentric (muscle lengthening and contracting) muscle contractions the system becomes efficient through these decelerating movements through the central nervous system enhanced visco-elastic rebound as well as the conservation of momentum. Hence, mogul skiing would need to generate this elastic rebound
see Motor Learning section for further explanations
Knee assessment and treatment using a motor control approach
The subjective examination should include aspects of the stage, stability, irritability and severity of the disorder.
Hence the physical examination should include analysis ofgait
squat
- pelvc symmetry
- lumbo-pelvic dynamics
- femoral pulse
- inferior lateral movements of the T/S and lateral diaphragm control over Psoas Major function
- foot dynamics (esp. pronation supination) - although the foot is in a boot during skiing, orthotic prescription for the boot may be advisable
- muscle timing and duration of contribution between Vastus Medialis and Vastus Lateralis, Gluteus Maximus and Hamstrings, Gluteus Medius and Adductor synergy, deep hip rotator endurance and strength.
- go to foot - orthotics section for further details
- Relationship between the deep and superficial abdominal muscles and their affect on pelvic symmetry and lumbopelvic rhythm.ROM's of the hip, knee, foot and L/S, medial stability of the knee can be assessed and treated using the following exercise
Rehabilitation through exercise
Lumbo-pelvic and hip dynamics can be assessed and treated using Muscle energy techniques
Cycling can be used to build up the muscles of the thigh and butt through optimal Cycling Kinematics
- Bike Seat Position
- anterior (front) knee pain : raise seat slightly (unless grossly malpositioned generally the changes are in the order of 2-3mm)
- posterior (back) knee pain : lower the seat slightly and/or move it forwards for butt tightness
- lateral (outside) knee pain : lower the seat and/or move it backwards
- inside knee pain : cleat and ankle position, symphasis pubis and adductor strain - seat may be too high, forefoot varus may require the insertion of a pedal wedge (Lemond LeWedges)
- Pedal Position

- moving the foot forward on the pedaal creates increases in quadriceps power, however it also increases the loading of the patello-femoral joint
- moving the foot back on the pedal engages the hamstrings and gluteal muscles to provide synergistic extensor power to the quadriceps
- Abdominal and Gluteal Strengthening

Knee Muscle representaion in the brain changes after injury
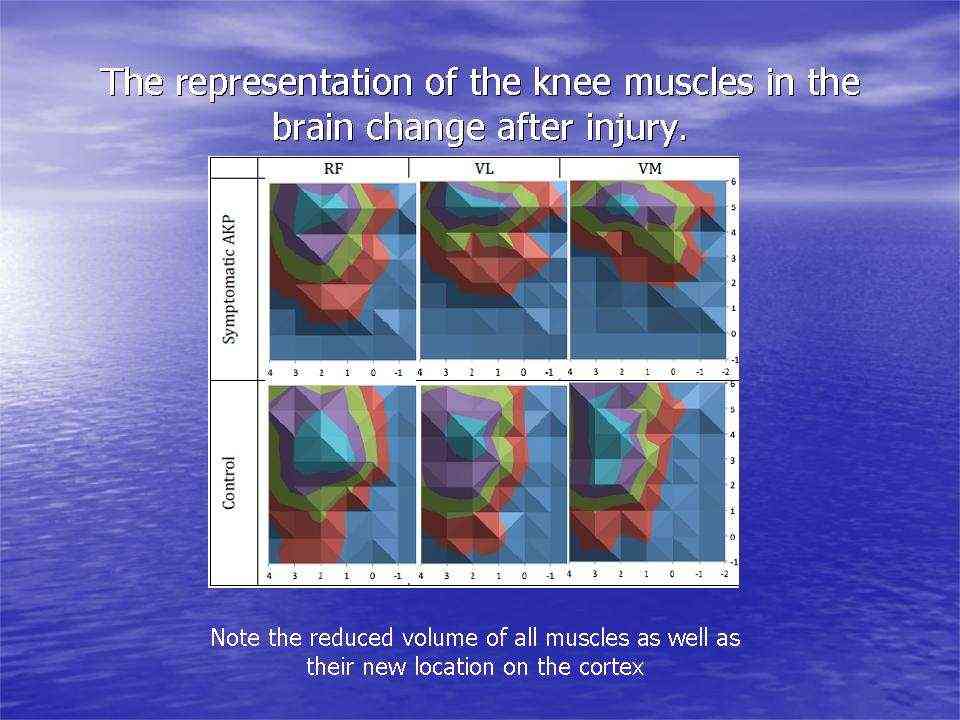
Transcortical muscle stimulation activity (Abrahao Fontes Baptista 2014)
-
Motor learning using Quadriceps VMO training

additionally, EMG can be used in combination with transverse abdominis, gluteus medius, medial calf muscles and VMO
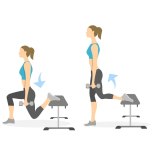
- Gluteal lengthening, combined quads/abdominal strengthening

- Lumbo-pelvic dynamic stretching a la Krause
Patella treatment using tape

Taping or other aids can also be used around the hip/buttocks to prevent femur internal rotation thereby reducing the relative lateral alignment of the patella w.r.t the femur.
Patella Tendonosis using an eccentric loading program
In conclusion, the examination and treatment of the knee for skiing should include assessment of all the structures which can affect knee function. Prior to the physical examination, a thorough subjective examination should be conduct to enable the client and the therapist to engage in the clinical reasoning process. Interested readers should look at the Instructional Design section of this website.

Last update : 17 June 2014